4150
Preliminary study of DCE-MRI combined with DWI in discriminating tumor deposits from lymph node metastasis in rectal cancer1The First Affiliated Hospital of Dalian Medical University, Dalian, China
Synopsis
Keywords: Diffusion/other diffusion imaging techniques, Cancer
Tumor deposits (TDs) in rectal cancer have been shown to be an important marker of poor prognosis. Although very similar to lymph node metastasis (LNMs), TDs have unique features in terms of biology and outcome, suggesting that distinguishing between these two entities may be of great importance. Results of this study indicate DWI and DCE-MRI can effectively differentiate TDs and LNMs in rectal cancer, Combination of DWI and DCE-MRI imaging may serve as an effective noninvasive method for differentiation of TDs from LNMs in rectal cancer.Introduction
Rectal cancer (RC) is one of the most common cancers and a leading cause of cancer-related death worldwide.1 Tumor deposits (TDs) in RC have been shown to be an important marker of poor prognosis.2 Conventional CT/MRI images cannot distinguish TDs from lymph node metastasis (LNMs) reliably. Unlike LNMs, TDs have unique features in terms of biology and outcome, suggesting that distinguishing between these two entities may be of great importance.3 Currently, the diagnosis of TDs still depends on the pathology after surgery, which is not conducive to the early evaluation of tumor characteristics. Thus, it is necessary to identify a non-invasive method that could accurately discriminating TDs from LNMs. Dynamic contrast-enhanced MRI (DCE-MRI) and Diffusion-weighted imaging (DWI) are helpful methods for the characterization of the pathophysiological features of tumors. DCE-MRI is a functional imaging that can provide valuable information about tumour aggressiveness and the degree of angiogenesis. DWI provides quantitative information about tumor cellularity.The purpose of this study is to explore the value of DCE-MRI and DWI in discriminating TDs from LNMs.Methods
This study has been approved by the local IRB. 31 patients with pathologically confirmed with rectal cancer were recruited in this study. The patients were divided into two groups: TDs group (15 patients) and LNMs group (16 patients). They underwent a examination on 3.0T MR (Signa HDxt, GE Medical Systems, USA) with a phased-array body coil. The MR sequences included T2WI, DWI, LAVA, etc. Detailed parameters were listed in Table 1.The original axial digital images from the DWI and DCE sequence were transmitted to the ADW 4.6 workstation. Functool software and GenIQ software were used to perform post-processing to obtain ADC and Ktrans, Kep,Ve maps, respectively. Two radiologists used a double-blind method to place three ROIs on the largest layer of the lesion to measure DCE parameters. The average values were calculated to minimize measurement bias. Mann-Whitney U test or Student’s t test was used to analyze the differences of ADC and DCE parameters between the two groups. The ROC curves were used to evaluate the diagnostic efficacy of these parameters in the differential diagnosis of the two groups.Results
The consistency of the data obtained by the two observers was good (ICC value > 0. 75). The Kep values of TDs group (1.50±0.64/min) were significantly lower than that of LNMs group (2.16±0.66/min) (P<0.05); the Ve [0.43(0.40,0.58) vs.0.32(0.21,0.47)] and ADC [1.18(1.06,1.33) vs.1.01(0.91,1.23)x10-3mm2/s] values of TDs group were significantly higher than those of LNMs group (P <0.05). The area under the ROC curve (AUC) for the ROC analyses of Kep, Ve and ADC for differentiation between TDs and LNMs groups was 0.773, 0.739, and 0.727, respectively. With combination of DWI and DCE parameters (Kep+Ve+ADC), the AUC of ROC analysis was improved to be 0.847.Discussion
The significant difference in ADC and DCE parameters between the two groups may be due to the more angiogenesis and higher cell density in rectal cancer patients with LNMs than in those with TDs. A combination of DWI and DCE parameters can greatly improve the differential diagnosis efficiency.Conclusion
Combination of DWI and DCE-MRI imaging is potentially a promising and valuable non-invasive method in differentiation of TDs from LNMs in rectal cancer.Acknowledgements
No acknowledgement found.References
1. Mattiuzzi C, Sanchis-Gomar F, Lippi G. Concise Update on Colorectal Cancer Epidemiology. Ann Transl Med. 2019;7(21):609.
2. Lord AC, D'Souza N, Pucher PH, et al. Significance of Extranodal Tumour Deposits in Colorectal Cancer: A Systematic Review and Meta-Analysis. Eur J Cancer. 2017;82:92–102.
3. Ueno H, Hashiguchi Y, Shimazaki H, et al. Peritumoral Deposits as an Adverse Prognostic Indicator of Colorectal Cancer. Am J Surg. 2014;207(1):70–7.
Figures
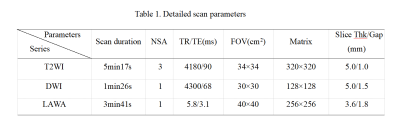
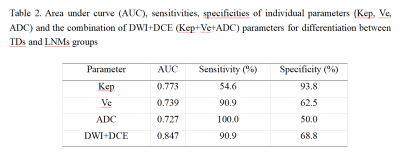
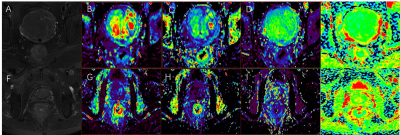
Figure 1. A 64-year-old male, rectal cancer with TDs. The T2WI(A), Ktrans (B), Kep(C), Ve(D) and ADC(E) maps were shown, Ktrans, Kep, Ve, and ADC values are 1.94/min, 1.05/min, 0.44, and 1.04×10-3 mm2 /s, respectively.
A 75-year-old male, rectal cancer with LNMs. The T2WI(F), Ktrans (G), Kep (H), Ve (I) and ADC(J) maps were shown, Ktrans, Kep, Ve, and ADC values are 0.76/min, 2.43/min, 0.32, and 0.97×10-3 mm2 /s, respectively.