4144
Predict late gadolinium enhancement using left ventricular long-axis strain in multiple myeloma with secondary cardiac amyloidosis patients1the Second Affiliated Hospital of Nanchang University, Nanchang, China, 2GE Healthcare, MR Research China, Beijing, China
Synopsis
Keywords: Cardiomyopathy, MR Value, Multiple myeloma; Cardiac amyloidosis; Long-axis strain
The purpose of this study was to evaluate the function of left ventricular (LV) in multiple myeloma (MM) with secondary cardiac amyloidosis (MM-CA) patients by cardiac magnetic resonance feature tracking (CMR-FT), and investigate the role of simple and fast CMR-FT long-axis strain (LAS) analysis in predicting late gadolinium enhancement (LGE). The results showed the LV function was more impaired in enhanced (LGE+) than in no-enhanced (LGE-) MM-CA patients. Among the investigated CMR-FT parameters, the LV LAS presented with best prediction efficacy of LGE. Our study indicated the simple and fast LAS may be beneficial for MM-CA patients with renal failure.Introduction
Multiple myeloma (MM) is a malignant disease with abnormal proliferation of clonal plasma cells[1]. It has been reported that up to 30% of MM patients can develop secondary amyloidosis[2]. MM patients with cardiac amyloidosis (CA) show poor prognosis with a median survival of only 6 months without intervention[3]. Late gadolinium enhancement (LGE) is one routinely used cardiac magnetic resonance (CMR) technique to diagnose CA in clinic. Previous studies have shown LGE can be used as predictor of major reverse events for CA patients[4-6]. However, MM with secondary CA (MM-CA) patients are often accompanied with renal amyloidosis which leads renal function insufficiency. LGE was limited to these patients in clinical practice.Global longitudinal strain (GLS) of CMR feature tracking (CMR-FT) shows incremental value of CA prognosis, but it requires substantial post-processing[7] . CMR-FT long-axis strain (LAS) is easier and faster than GLS and has been used to quantitatively evaluate the impairment of left ventricular (LV) function [7, 8]. The purpose of this study was to evaluate the LV function in MM-CA patients and investigate the possibility to predict LGE using LAS.
Material and Methods
Subjects33 MM-CA patients were retrospectively selected in this study. All participants didn’t have renal failure.
MRI experiment
All CMR imaging were performed using 3.0 Tesla scanner (Discovery MR750W; GE Healthcare, Milwaukee, CA, USA) using an 8-channel heart phased array coil. Fast balanced steady-state free-feed sequence was used to acquire the short-axis, two-chamber, three-chamber, and four-chamber heart cine images with the following parameters: TR 3.9 ms; TE 1.6 ms; FOV 38cm×38cm; reconstruction matrix: 256×256; flip angle 55°; slice thickness 6mm. For LGE, the short-axis, two-chamber and four-chamber heart were scanned 5-8 min later after intravenous injection of gadolinium.
Data analysis
The CMR original images were transferred into the CVI (Circle Cardiovascular Imaging, Inc., Calgary, Canada) software for post-processing. The multiplanar long-axis functional module was applied to delineate the epicardial contours of the left ventricle in two-chamber and four-chamber heart cine images using an automatic tracking technique to extract the left ventricular function parameters (Figure 1), including end-diastolic volume index (EDVI), end-systolic volume index (ESVI), stroke volume index (SVI), left ventricular ejection fraction (LVEF), cardiac output (CO), cardiac index (CI), left ventricle mass index (LVMI) and LV LAS. The LGE images were visually evaluated for the presence or absence of delayed enhancement pattern. The patients with and without LGE were group as LGE+ and LGE-, respectively.
The R and MedCalc software were used for statistical analysis. Categorical data were compared using either Chi-square test or Fisher's exact test. The count data were tested by Shapiro-Wilk test. Non-normally distributed data were compared using the Kruskal-Wallis rank sum test. The Mann-Whitney U test was used for the comparison between groups of nonparametric quantitative data. The receiver operating characteristics (ROC) analysis was carried out to evaluate the performance of LGE prediction. Area under curve (AUC) was used present the prediction efficacy. The P<0.05 was considered as statistically significant.
Results
Among the selected patients, 21 patients were LGE+ and the other 12 patients were LGE-. The CMR cine images showed that the myocardium thickness was uniform (Fig.2 A and E) and both atriums were enlarged (Fig.2 B and F) in all MM-CA patients. For the LGE+ patients, diffuse subendocardial enhancement (Fig.2 C) and partial transmural enhancement (Fig.2 D) can be observed. However, no obvious enhancement can be observer in LGE- patients (Fig.2 G and H).As shown in Table 1, the LGE+ patients presented with worse LV function as indicated by significantly lower LVEF (50.02% vs 63.83%; P < 0.001) and CI (2.60 vs 3.62; P = 0.025) and larger LVMI (95.6 vs 62.57; P < 0.001). LAS also suggested the LV was significantly more impaired in LGE+ patients (-8.19 vs -15.95; P<0.001).
As shown in Fig. 3, the CI provided moderate prediction efficacy of LGE (AUC=0.738). The prediction efficacy was better using LVEF (AUC=0.865) and LVMI (AUC=0.877) compared with CI. Among these predictors, LV LAS presented the best prediction efficacy (AUC=0.909).
Discussion and Conclusion
In this study, CMR-FT was used to evaluate the LV function in MM-CA patients. The results revealed the LGE+ MM-CA patients showed more impaired LV function compared with LGE- ones. Among the predictive parameters derived from CMR-FT, the LV LAS presented with the best prediction efficacy (AUC=0.909).It has been reported about 69%-80% CA patients presented with LGE+[9, 10] . Our results showed a relatively lower LGE+ ratio in MM-CA patients (i.e., 64%). Perugini[9] had reported ESVI was correlated with global enhancement score in CA patients. However, we didn’t find significant difference ESVI between LGE+ and LGE- MM-CA patients. Instead, the CI, LVEF, LVMI, and LV LAS were significantly different between the two subgroups of MM-CA patients and can be used to predict LGE.
In conclusion, CMR-FT can be used to evaluate the LV function of MM-CA patients. The simple and fast LV LAS analysis can be used to predict LGE+ and LGE- and can be beneficial for MM-CA with renal failure patients.
Acknowledgements
None.References
1. Singh G, Savage NM, Jillella AP, et al. Light Chain-Predominant Multiple Myeloma Subgroup: Impaired Renal Function Correlates with Decreased Survival. Lab Med. 2022 Mar 7;53(2):145-148.
2. Siddiqi OK, Ruberg FL. Cardiac amyloidosis: An update on pathophysiology, diagnosis, and treatment. Trends Cardiovasc Med. 2018 Jan;28(1):10-21.
3. Cariou E, Bennani Smires Y, Victor G, et al. Diagnostic score for the detection of cardiac amyloidosis in patients with left ventricular hypertrop hy and impact on prognosis. Amyloid. 2017;24(2):101-109.
4. Bhatti S, Watts E, Syed F, et al. Clinical and prognostic utility of cardiovascular magnetic resonance imaging in myeloma patients with suspected cardiac amyloidosis. Eur Heart J Cardiovasc Imaging. 2016 Sep;17(9):970-977.
5. Wan K, Sun J, Yang D, et al. Left Ventricular Myocardial Deformation on Cine MR Images: Relationship to Severity of Disease and Prognosis in Light-Chain Amyloidosis. Radiology. 2018 Jul;288(1):73-80.
6. Li X, Li J, Lin L, et al. Left and right ventricular myocardial deformation and late gadolinium enhancement: incremental prognostic value in amyloid light-chain amyloidosis. Cardiovasc Diagn Ther. 2020 Jun;10(3):470-480.
7. Schuster A, Backhaus SJ, Stiermaier T, et al. Fast manual long-axis strain assessment provides optimized cardiovascular event prediction following myocardial infarction. Eur Heart J Cardiovasc Imaging. 2019 Nov 1;20(11):1262-1270.
8. Riffel JH, Andre F, Maertens M, et al. Fast assessment of long axis strain with standard cardiovascular magnetic resonance: a validation study of a novel parameter with reference values. J Cardiovasc Magn Reson. 2015 Aug 8;17:69.
9. Perugini E, Rapezzi C, Piva T, et al. Non-invasive evaluation of the myocardial substrate of cardiac amyloidosis by gadolinium cardiac magnetic resonance. Heart. 2006;92(3):343-349.
10. Vogelsberg H, Mahrholdt H, Deluigi CC, et al. Cardiovascular magnetic resonance in clinically suspected cardiac amyloidosis: noninvasive imaging compared to endomyocardial biopsy. J am coll cardiol. 2008;51(10):1022-1030.Figures
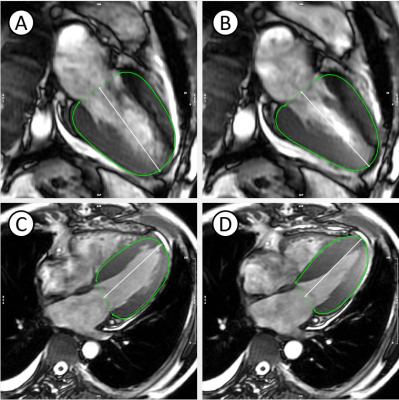
Fig. 1 LV LAS post-processing diagram. At the end diastolic and end-systolic phases of the left ventricle, the length of the shortening of the midpoint of the epicardial apical boundary and the beginning of the anteromedial and posterolateral lobes of the mitral valve was measured, and the LAS of the two (A and B) and four (C and D) chambers during myocardial contraction was evaluated.
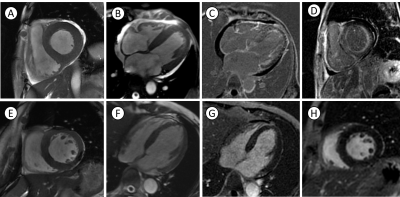
Fig. 2 Typical CMR findings in patients with CA secondary to MM. Upper row LGE+ patient: left ventricular myocardial homogeneous thickening(A); bi-atria enlargement(B); LGE sequence shows diffuse subendocardial circumferential enhancement at the level of the four-chambered heart with pericardial cavity effusion(C); partial myocardial transmural enhancement of the left ventricle at the short-axis level of the LGE sequence(D). Lower row LGE- patient: homogeneous thickening of the myocardium (E and F); no abnormal enhancement of LGE sequence (G and H).
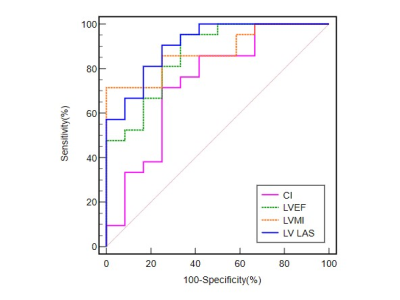
Table. 1 Comparisons of LV cardiac function parameters of CMR between subgroups
Abbreviations: EDVI: end-diastolic volume index; ESVI: end-systolic volume index; SVI: stroke volume index; LVEF: left ventricular ejection fraction; CO: cardiac output; CI: cardiac index; LVMI: left ventricle mass index; LV LAS: left ventricular long-axis strain.