4127
A nomogram based on IVIM-DWI and Clinical parameters to Predict Survival of Rectal Cancer Patients after Radical Resection
Haodong Jia1
1Anhui Provincial Hospital Affiliated to Anhui Medical University, Hefei, China
1Anhui Provincial Hospital Affiliated to Anhui Medical University, Hefei, China
Synopsis
Keywords: Pelvis, fMRI
This is an abstract by Haodong Jia.
Objectives
To explore the value of the nomogram based on IVIM-DWI and clinical parameters for predicting survival in rectal cancer patients after radical resection.Subjects and Methods:
This was a retrospective analysis of 101 patients (61 males and 40 females) with rectal cancer treated with radical resection, between January 2015 and June 2020. The IVIM-DWI quantitative parameters (ADC, D, D*, f) and clinical parameters of all patients were measured and collected. Cox regression analysis was used to construct a nomogram for predicting disease-free survival (DFS) and overall survival (OS) in rectal cancer patients after radical resection, and performance of the model was assessed by concordance indexes (c-index).Results
Results: Age, D value, CA19-9 and lymph node metastasis (LNM) were independent prognostic factors for OS in rectal cancer patients after radical resection, and their HR were 1.041, 0.083, 3.393 and 4.141, respectively. The f values and CA19-9 were independent prognostic factors for DFS in rectal cancer patients after radical resection, and their HR was 17.537 and 2.788, respectively. The area under the curve (AUC) of the 1-year, 3-year and 5-year DFS and OS predicted by the model was 0.798, 0.762, 0.843 and 0.891, 0.788, 0.875, respectively, and the c-index was 0.733 and 0.774.Conclusion
The nomogram based on IVIM-DWI values and clinical parameters had high clinical value in predicting DFS and OS in rectal cancer patients with radical resection, and could be used as a prognostic marker for rectal cancer patients.Acknowledgements
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.References
[1] Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin. 2018, 68(6):394-424. DOI: 10.3322/caac.21492.[2] Plodeck V, Rahbari NN, Weitz J, Radosa CG, et al. FDG-PET/MRI in patients with pelvic recurrence of rectal cancer: first clinical experiences[J]. Eur Radiol. 2019, 29(1):422-428. DOI: 10.1007/s00330-018-5589-6.[3] Li Q, Dai W, Li Y, Xu Y, Li X, Cai S. Nomograms for predicting the prognostic value of serological tumor biomarkers in colorectal cancer patients after radical resection[J]. Sci Rep. 2017 Apr 18;7:46345. DOI: 10.1038/srep46345. [4] Reggiani Bonetti L, Lionti S, Domati F, et al. Do pathological variables have prognostic significance in rectal adenocarcinoma treated with neoadjuvant chemoradiotherapy and surgery?[J] World J Gastroenterol 2017,23(8):1412-1423. DOI: 10.3748/wjg.v23.i8.1412. [5] Le Bihan D, Breton E, Lallemand D, et al. Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology 1988;168:497-505. DOI: 10.1148/radiology.168.2.3393671.[6] Pijnappel EN, Wassenaar NPM, Gurney-Champion OJ, et al. Phase I/II Study of LDE225 in Combination with Gemcitabine and Nab-Paclitaxel in Patients with Metastatic Pancreatic Cancer. Cancers (Basel). 2021,13(19):4869. DOI: 10.3390/cancers13194869.[7] Yu XP, Wen L, Hou J, et al. Discrimination between Metastatic and Nonmetastatic Mesorectal Lymph Nodes in Rectal Cancer Using Intravoxel Incoherent Motion Diffusion-weighted Magnetic Resonance Imaging[J]. Acad Radiol. 2016, 23(4):479-485. DOI: 10.1016/j.acra.[8] Zhang F, Zhang Y, Zhao W, et al. Metabolomics for biomarker discovery in the diagnosis, prognosis, survival and recurrence of colorectal cancer: a systematic review[J]. Oncotarget. 2017,8(21):35460-35472. DOI:10.18632/oncotarget.16727.[9] Luo G, Liu C, Guo M, et al. Potential Biomarkers in Lewis Negative Patients With Pancreatic Cancer[J]. Ann Surg. 2017,265(4):800-805. DOI: 10.1097/SLA.0000000000001741. [10] Sun ZQ, Ma S, Zhou QB, et al. Prognostic value of lymph node metastasis in patients with T1-stage colorectal cancer from multiple centers in China[J]. World J Gastroenterol. 2017,23(48):8582-8590. DOI:10.3748/wjg.v23.i48.8582.[11] Bengulescu I, Radu P, Iorga C, Bratucu M, et al. The Value of Endoscopy as a Predictive Factor when Evaluating the Clinical Response to Neoadjuvant Chemoradiotherapy for Patients with Rectal Cancer. Chirurgia (Bucur)[J]. 2020,115(3):373-379. DOI: 10.21614/chirurgia.115.3.373. [12] Li Destri G, Maugeri A, Ramistella A, et al. The prognostic impact of neoadjuvant chemoradiotherapy on lymph node sampling in patients with locally advanced rectal cancer[J]. Updates Surg. 2020,72(3):793-800. DOI: 10.1007/s13304-020-00841-3. [13] Parisi A, Cortellini A, Venditti O, et al. Family History of Cancer as Potential Prognostic Factor in Stage III Colorectal Cancer: a Retrospective Monoinstitutional Study[J]. J Gastrointest Cancer. 2020,51(3):1094-1101. DOI: 10.1007/s12029-020-00452-6. [14] Zaborowski A, Stakelum A, Winter DC. Systematic review of outcomesafter total neoadjuvant therapy for locally advanced rectal cancer[J]. Br.J. Surg. 2019, 106(8): 979-987. DOI: 10.1002/bjs.11171.[15] Allemani C, Weir HK, Carreira H, et al. Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries(CONCORD-2)[J].Lancet.2015,385(9972):977-1010.DOI:10.1016/S0140-6736(14)62038-9.[16] Maeda K, Shibutani M, Otani H, et al. Inflammation-based factors and prognosis in patients with colorectal cancer[J]. World J Gastrointest Oncol. 2015,7(8):111-7. DOI: 10.4251/wjgo.v7.i8.111.[17] Fan S, Li T, Zhou P, et al. Development and validation of nomogram combining serum biomarker for predicting survival in patients with resected rectal cancer[J]. Biosci Rep. 2019 Nov 29;39(11):BSR20192636. DOI: 10.1042/BSR20192636.[18] Zeng Q, Hong Y, Cheng J, et al. Quantitative study of preoperative staging of gastric cancer using intravoxel incoherent motion diffusion-weighted imaging as a potential clinical index[J]. Eur J Radiol. 2021,141:109627. DOI: 10.1016/j.ejrad.2021.109627. [19] Zhu Y, Jiang Z, Wang B, et al. Quantitative Dynamic-Enhanced MRI and Intravoxel Incoherent Motion Diffusion-Weighted Imaging for Prediction of the Pathological Response to Neoadjuvant Chemotherapy and the Prognosis in Locally Advanced Gastric Cancer[J]. Front Oncol. 2022,12:841460. DOI: 10.3389/fonc.2022.841460. [20] Zhang F, Zhang Y, Zhao W, et al. Metabolomics for biomarker discovery in the diagnosis, prognosis, survival and recurrence of colorectal cancer: a systematic review[J]. Oncotarget. 2017,8(21):35460-35472. DOI:10.18632/oncotarget.16727. [21] Massacesi C, Norman A, Price T, et al. A clinical nomogram for predicting long-term survival in advanced colorectal cancer[J]. Eur J Cancer. 2000,(16):2044-2052. DOI: 10.1016/s0959-8049(00)00286-0. [22] Park MY, Park IJ, Ryu HS, et al. Optimal Postoperative Surveillance Strategies for Colorectal Cancer: A Retrospective Observational Study. Cancers (Basel)[J]. 2021,13(14):3502. DOI: 10.3390/cancers13143502. [23] Liu Z, Meng X, Zhang H, et al. Predicting distant metastasis and chemotherapy benefit in locally advanced rectal cancer[J].Nat Commun. 2020,11(1):4308. DOI: 10.1038/s41467-020-18162-9. [24] Zhou Y, Yang G, Gong XQ, et al. A study of the correlations between IVIM-DWI parameters and the histologic differentiation of hepatocellular carcinoma. Sci Rep. 2021 May 17;11(1):10392. doi: 10.1038/s41598-021-89784-2. PMID: 34001962; PMCID: PMC8129092.[25] Le Bihan D, Breton E, Lallemand D, et al. MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders[J]. Radiology,1986,161(2):401-407. DOI: 10.1148/radiology.161.2.3763909. [26] Woo S, Lee JM, Yoon JH, et al. Intravoxel incoherent motion diffusion-weighted MR imaging of hepatocellular carcinoma: correlation with enhancement degree and histologic grade[J]. Radiology. 2014 Mar;270(3):758-67. DOI: 10.1148/radiol.13130444. [27] Sun H, Xu Y, Song A, et al. Intravoxel Incoherent Motion MRI of Rectal Cancer: Correlation of Diffusion and Perfusion Characteristics With Prognostic Tumor Markers[J]. AJR Am J Roentgenol. 2018,210(4):W139-W147. DOI: 10.2214/AJR.17.18342. [28] Watanabe H, Kanematsu M, Goshima S, et al. Characterizing focal hepatic lesions by free-breathing intravoxel incoherent motion MRI at 3.0 T[J]. Acta Radiol. 2014,55(10):1166-1173. DOI: 10.1177/0284185113514966. [29] Kanakis G, Kaltsas G. Biochemical markers for gastroenteropancreatic neuroendocrine tumours (GEP-NETs)[J]. Best Pract Res Clin Gastroenterol, 2012,26(6):791-802. DOI: 10.1016/j.bpg.2012.12.006.[30] Luo G, Liu C, Guo M, et al. Potential Biomarkers in Lewis Negative Patients With Pancreatic Cancer[J]. Ann Surg. 2017,265(4):800-805. DOI: 10.1097/SLA.0000000000001741. [31] Wang J, Wang X, Yu F, et al. Combined detection of preoperative serum CEA, CA19-9 and CA242 improve prognostic prediction of surgically treated colorectal cancer patients[J]. Int J Clin Exp Pathol, 2015,8(11):14853-14863.[32] Basbug M, Arikanoglu Z, Bulbuller N, et al. Prognostic value of preoperative CEA and CA 19-9 levels in patients with colorectal cancer. Hepatogastroenterology. 2011,58(106):400-405. [33] Vukobrat-Bijedic Z, Husic-Selimovic A, Sofic A, Bijedic N, Bjelogrlic I, Gogov B, Mehmedovic A. Cancer Antigens (CEA and CA 19-9) as Markers of Advanced Stage of Colorectal Carcinoma[J]. Med Arch. 2013,67(6):397-401. DOI:10.5455/medarh.2013.67.397-401.[34] Takakura Y, Ikeda S, Imaoka Y, Urushihara T, Itamoto T. An elevated preoperative serum carbohydrate antigen 19-9 level is a significant predictor for peritoneal dissemination and poor survival in colorectal cancer[J]. Colorectal Dis. 2015,17(5):417-25. DOI: 10.1111/codi.12865. [35] Selcukbiricik F, Bilici A, Tural D, et al. Are high initial CEA and CA 19-9 levels associated with the presence of K-ras mutation in patients with metastatic colorectal cancer?[J] Tumour Biol. 2013,34(4):2233-2239. DOI: 10.1007/s13277-013-0763-6.[36] Takada A, Ohmori K, Takahashi N, Tsuyuoka K, et al. Adhesion of human cancer cells to vascular endothelium mediated by a carbohydrate antigen, sialyl Lewis A[J]. Biochem Biophys Res Commun. 1991,179(2):713-719. DOI: 10.1016/0006-291x(91)91875-d. [37] Manceau G, Karoui M, Werner A, et al. Comparative outcomes of rectal cancer surgery between elderly and non-elderly patients:a systematic review[J]. Lancet Oncol. 2012 13(12):e525-36. DOI: 10.1016/S1470-2045(12)70378-9.Figures
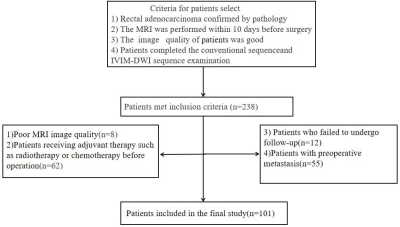
Flowchart of prediction of survival based on IVIM-DWI and clinical parameters in rectal cancer patients after radical resection.

(a-e) MR images of a 55-year-old man in the survival group with moderate degree of differentiation rectal adenocarcinoma. (a): DWI showed that primary lesion of rectal adenocarcinoma presented with hyperintensity. (b)apparent diffusion coefficient (ADC) map;(c)diffusion coefficient (D) map;(d)pseudo diffusion coefficient (D*) map; (e)microvascular volume fraction (f) map.(f-j) (f): DWI map. (g)ADC map;(h)D)map;(i)D*map;(j)f map. MR images of a 68-year-old man in the death group with moderate degree of differentiation rectal adenocarcinoma.
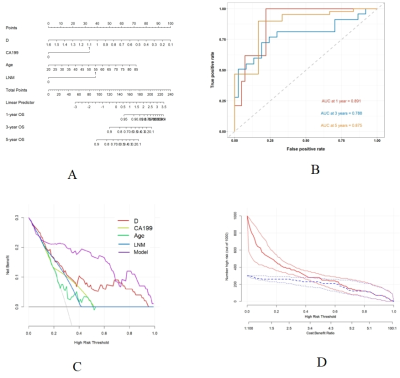
Nomograms and its ROC curves, decision curves and clinical impact curves for predicting OS in rectal cancer patients after radical resection.
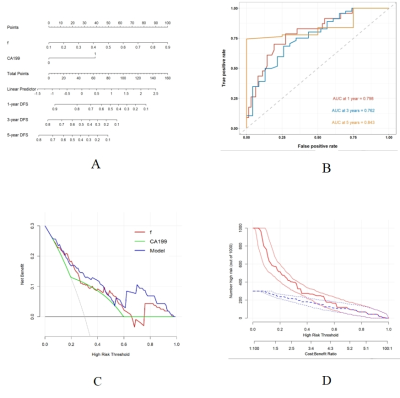
Nomograms and its ROC curves, decision curves and clinical impact curves for predicting DFS in rectal cancer patients after radical resection.
DOI: https://doi.org/10.58530/2023/4127