4122
Clinical value of DWI combined with APT in differentiating rectal cancer from non-rectal cancer1Shaanxi Provincial People's Hospital, XI'AN, China, 2Philips Healthcare, XI'AN, China
Synopsis
Keywords: Cancer, Diffusion/other diffusion imaging techniques
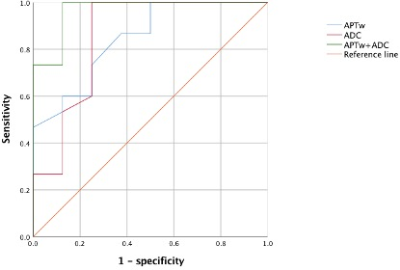
We aimed to explore the diagnostic value of amide proton transfer-weighted (APTw) imaging combined with diffusion-weighted imaging (DWI) in differentiating rectal cancer from non-rectal cancer. The result showed that, compared with APTw or DWI (AUC=0.846 and 0.854, respectively), the highest diagnostic efficacy (AUC=0.967) was acquired using APTw combined with apparent diffusion coefficient (ADC) values.Introduction
Rectal cancer is one of the leading causes of cancer-related deaths worldwide, accounting for 30% of all colorectal cancers [1]. MRI has gradually become an important imaging technology for diagnosis and evaluation of rectal cancer due to the high soft tissue resolution [2]. Amide proton transfer-weighted (APTw)imaging technology can provide the information of high revolution free protein and amino compound proton of peptide in vivo to reflect the distribution of protein in tumor and aid in tumors’ grading and staging [3].Diffusion-weighted imaging (DWI) is well-established noninvasive technique to detect the diffusion of water molecules in tissues. It can be used to investigate tissue organization, structural and functional status of a biological object at the cellular and molecular level. DWI derived apparent diffusion coefficient (ADC) map has been a quantitative measurement for differentiation of benign and malignant rectal cancers [4]. In this study, we aim to explore the diagnostic value of APTw, DWI and their combinationin differentiating rectal cancer from non-rectal cancer.Materials and Methods
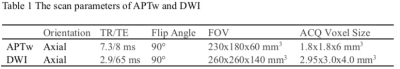
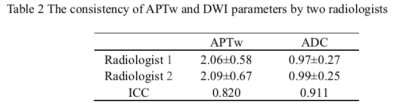
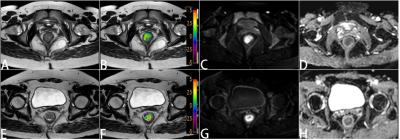
Twenty-three patients (average age of 60.3± 10.5years, 11females and 12males) with rectal tumor underwent MR examination for DWI and APTw on a 3.0T MR (Ingenia CX, Philips,the Netherlands). None of them received neoadjuvant therapy before examinations. According to the pathological results, they were divided intorectal cancer (15 patients) and non-rectal cancer (8 patients) groups. APTw and DWI images were transferred to Philips Intellispace Portal workstation for post-processing. The scan parameters were shown in Table 1. The ADC and APTw values of the rectal tumors were measured by two radiologists (Fig 1). Three circular ROIs were placed along the periphery of the tumor at the level of the largest area of the mass and taking the mean value of them. Artifacts, blood vessels, regions of necrosis, and tumor stalk were avoided. The ADC and APTw value between two groups were compared. Intra-group correlation coefficient (ICC) was used to test the consistency of the two radiologists' measurements. The difference in parameters was analyzed by independent samples T test, and the diagnostic efficacy was evaluated by ROC analysis. The diagnostic efficacy of ADC, APTw and ADC combined with APTw was analyzed by logistic regression.Results
APTw combined with DWI derived ADC map can effectively differentiate rectal tumors from non-rectal tumors. It can provide a promising method for rectal tumor diagnosis and prognosis.The demographic and clinical characteristics of twenty-three patients with rectal tumor were fifteen rectal adenocarcinoma patients and eight non-rectal cancer patients (neuroendocrine tumors 1, stromal tumor 1 and rectal adenomata 6). The consistency of the measurements obtained by the two observers were good (ICC value > 0.8, Table 2). The value of APTw in rectal cancer group was higher than that of non- rectal cancer group, and the value of ADC in non-rectal cancer group was higher than that of rectal cancer group, with statistically significant difference (P < 0.05, Table 3). Area under the curve (AUC) for APTw and ADC to rectal cancer form non-rectal cancer were 0.846 and 0.854, respectively. The sensitivity of above parameters corresponding to their respective feasible threshold values were 86.7% and 100 %, and the specificity were 62.5% and 75%, respectively. With APTw values combined with ADC, we found that the diagnostic efficacy was significantly higher in both groups (AUC=0.967, sensitivity=100% and specificity=87.5%, Fig 2).Discussion
APTw imaging combined with DWI has a high value in differentiating rectal tumors. Among the single parameter, the diagnostic efficacy of ADC was the highest (AUC=0.854). When APTw values combined withADC values, the diagnostic efficacy was significantly improved (AUC=0.967). APTw imaging can contribute to the differentiating rectal cancer from non-rectal cancer which possess different water-exchangeable chemical groups and tissue physicochemical properties. Compared with non-rectal cancer, the ADC values of rectal cancer was smaller due to higher density of tissue cells in rectal cancer greatly restricting water molecule diffusion. Clinically, DWI can be used in the differentiation of benign and malignant tumors. ADC value is affected by b value, while APTw is not. Rectal cancer produces more free proteins and peptides synthesized and APTw is beneficial for improving the results of DWI and provides additional information.Conclusion
APTw combined with DWI derived ADC map can effectively differentiate rectal tumors from non-rectal tumors. It can provide a promising method for rectal tumor diagnosis and prognosis.Acknowledgements
No acknowledgement foundReferences
[1]Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin 2020;70(1):7-30
[2] KSAR Study Group for Rectal Cancer. Essential items for structured reporting of rectal cancer MRI: 2016 consensus recommendation from the Korean Society of Abdominal Radiology. Korean J Radiol 2017;18:132-151
[3] Nishie A, Takayama Y, Asayama Y, et al. Amide proton transfer imaging can predict tumor grade in rectal cancer. Magn Reson Imaging. 2018;51:96-103.2018.04.017
[4] Chandramohan A, Siddiqi U M, Mittal R, et al. Diffusion weighted imaging improves diagnostic ability of MRI for determining complete response to neoadjuvant therapy in locally advanced rectal cancer[J]. European Journal of Radiology, 2020, 7(7)
Figures