4098
Lung Multi-Breath Wash in/out MRI with 19F with Sub 0.5 Second Scan Time
Sang Hun Chung1, Khoi Minh Huynh1, Yong Chen2, Pew-Thian Yap1, Jennifer Goralski1, Scott Donaldson1, and Yueh Z Lee1
1University of North Carolina Chapel Hill, chapel hill, NC, United States, 2Case Western Reserve University, Cleveland, OH, United States
1University of North Carolina Chapel Hill, chapel hill, NC, United States, 2Case Western Reserve University, Cleveland, OH, United States
Synopsis
Keywords: Data Acquisition, Lung, 19F fluorine
We studied the feasibility of multi breath wash-in/out lung acquisition with 19F gas and a sub 0.5 second acquisition spiral sequence. We compared the sub 0.5 seconds acquired data ability to measure wash-in/out time constants to a regular breath-hold 19F lung imaging and report correlation as well as differences in mean. Our results yielded high correlations (r > 0.88) for both wash-in and wash-out time constant calculations. The results indicate our proposed method yield similar calculated time wash-in/out time constants without the need for breath-holds and show promise for the use of free breathing 19F gas lung MRI.Introduction
Analysis of multi-breath wash-in wash-out (MBWW) MRI has been shown to provide a marker of lung disease more sensitive than the current gold standard percent predicted forced expiratory volume (ppFEV1)1. However, MBWW commonly requires patients to hold their breaths during the scans, which makes the study of children (<5 years) and patient with high disease progression difficult. 19F has features that make it suitable for MBWW study over other commonly used contrast agents like 129Xe and 3He such as it being used without hyperpolarization and it being storable at large volumes premixed in a normoxing mixture of 21% O2, 79 % 19F. In this abstract we study the feasibility of sub 0.5 seconds (suitable for free breathing) scans during MBWW.Methods
MRI images were acquired using a multinuclear-capable Prisma 3.0T scanner (Siemens Medical Systems, Erlangen, Germany) and a custom 8-channel transmit/receive 19F-tuned chest coil (ScanMed, Inc., Omaha NE). 3 healthy and 8 Cystic Fibrosis (CF) individuals participated in this study. Percent predicted forced expiratory volume (ppFEV1) was measured for each participant prior to MR scanning on the same day.1H MRI scans were acquired for each participant using 3D Fast Low Angle (FL3D) based ultra-short echo time (UTE) while breath-holding for later masking 19F images (TE/TR 0.05/2.42 ms, FA 5o, resolution 2.14X2.14x2.5 mm, number of slices 103, scan time 17 seconds).For 19F acquisition, the participants underwent 10 wash-in breaths, they were instructed to perform deep inhalations every other breath and breath-hold for the duration of the scans. During the breath-hold, a Volumetric interpolated breath-hold examination (VIBE) sequence (TE/TR 1.61/13 ms, FA 74o, resolution 6.25X6.25x15 mm, number of slices 18, scan time 18 seconds) followed by a 4 arm spiral sequence images (TE/TR 0.48/11 ms, FA 74o, resolution 6.25X6.25x15 mm, number of slices 18, scan time 0.45 seconds) were acquired. Wash-out imaging was performed in a similar way while participant’s inspiration gas was returned to room air until no 19F signal was visible.
The VIBE 19F Maximum intensity image (MIP) was registered to the 1H UTE and a mask was drawn over the thoracic cavity. The spiral images were denoised2 and registered to the 19F images (translation only). The previously drawn lung mask was used to analyze both 19F VIBE and 19F spiral images. The mean signal inside the whole lung was computed for both 19F method and fitted to a biexponential curve to calculate the wash-in time constant (Tau1) and wash-out time constant (Tau1). MBWW of the lung mean was compared between the two methods for signal intensity, and time constants using Bland-Altman plots.
Results
Good agreement was found between the 19F VIBE and 19F Spiral MBWW analysis. Table 1 shows the participants CF state. Figure 1 shows an example VIBE and Spiral coronal screenshots with all participant aggregated mean signals at the bottom of each method. Signal intensity had a high correlation coefficient (r) value of 0.99 (difference in mean of 0.007, p=0.01, Figure 2), the MBWW time constants had r values of 0.83 (Tau1, difference in mean of -1.16, p=0.70, Figure 3) and 0.87 (Tau2, difference in mean of -1.54, p=0.11, Figure 4).Discussion
The spiral scans are seen to be linearly proportional in signal to the VIBE scans based on Figure 2. Z-score normalization was used due to the denoising process changing the absolute magnitudes. The r values were good for the MBWW time constants Tau1 (r = 0.83) and tau2 (r = 0.87) which show promise of performing MBWW with only the spiral scans. The Bland-Altman difference in mean values were small; -1.16 (Tau1, p = 0.70) and -1.54 (Tau2, p = 0.11), strengthening the feasibility for very short breath-holds or free breathing 19F dynamic lung MRI.The low number of subjects is a limitation of this study; we are currently recruiting additional subjects and expect more data points to yield significant time constant p-values. Further analysis is planned for comparison of MBWW metrics on a voxel-by-voxel basis, which will give us both temporal as well as spatial information. Looking forward, we anticipate that further comparisons between full inhalation and tidal volume breathing are also needed.
Conclusion
Good agreement was shown between 19F MBWW comparison between the breath-hold requiring VIBE sequence (scan time 18 seconds) to the short spiral sequence (scan time 0.45 seconds). MBWW parameters shower good correlation (signal r=0.99, wash-in Tau1 r=0.83, and wash-out r=0.87), suggesting the utility of this approach for the quantitative assessment of lung ventilation.Acknowledgements
This work was supported by the Cystic Fibrosis Foundation (PROMISE-MCC18K0; GORALS19Y5) and the National Institute of Health (K23-HL138257-01A1; P30 DK065988)References
1. Goralski JL, Chung SH, Glass TM, Ceppe AS, Akinnagbe-Zusterzeel EO, Trimble AT, et al. Dynamic perfluorinated gas MRI reveals abnormal ventilation despite normal FEV1 in cystic fibrosis. JCI Insight 2020;5(2):e133400.
2. Huynh KM, Chang WT, Chung SH, Chen Y, Lee Y, Yap PT. Noise mapping and removal in complex-valued multi-channel MRI via optimal shrinkage of singular values. International Conference on Medical Image Computing and Computer-Assisted Intervention. September 27, 2021; pp. 191-200. Springer, Cham.
Figures
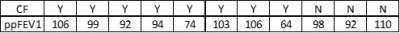
Table 1. CF status
and ppFEV1
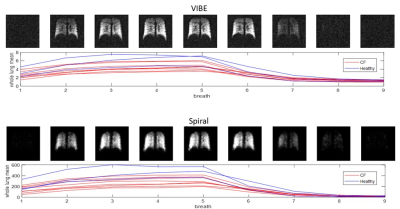
Figure 1. Example
coronal slice view of one participant of VIBE (top) and Spiral (bottom) for
wash-in (breaths 1-5) and wash-out (breaths 6-9). The corresponding breath mean
signal is plotted for all participants, CF participants are shown in red and healthy
participants are shown in blue

Figure 2. Z-score normalized mean intensity values of all data points from VIBE and spiral scans
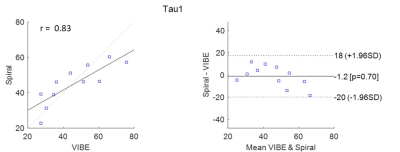
Figure 3. Wash-in time constant (Tau1) between VIBE and spiral scans

Figure 4. Wash-out time constant (Tau2) between VIBE and spiral scans
DOI: https://doi.org/10.58530/2023/4098