3994
Multiparametric Cardiac Magnetic Resonance Reveals Persistent Myocardial injury in Patients with Exertional Heat illness1Jinling Hospital, Medical School of Nanjing University, Nanjing, China, 2GE Healthcare, Bei Jing, China
Synopsis
Keywords: Inflammation, Cardiovascular
To explore the clinical potential of multiparametric cardiac magnetic resonance (CMR) in evaluating myocardial injury in patients with exertional heat illness (EHI).This prospective study enrolled 28 male with EHI and 18 age-matched male healthy controls. All subjects underwent CMR, and 9 patients had follow-up CMR measurements 3 months after recovery from EHI. As shown in this study, EHI patients have left ventricular dysfunction, myocardial edema and fibrosis, and persistent myocardial injury at 3-month follow-up after the EHI episode. This knowledge has an important role in guiding patients recovering from EHI back to a return to work, play or duty, respectively.Introduction
Climate change has contributed to a paradigm shift in the lives of people with more episodes of heat illnesses and a high burden of death contributed to strong heat impacts [1]. Exertional heat illnesses (EHI) usually occurs in young and healthy individuals, such as military personnel [2], workers and athletes who participate in heavy tournaments at hot temperatures [3,4]. The cardiovascular system is a vital target organ to heat injury. It has been reported that the incidence of myocardial injury is as high as 43.4 - 65.2% [5, 6] and plays an important role on the death of patients with severe EHI among those who have experienced prior hospitalization for heat illness [7]. In recent years, cardiac magnetic resonance (CMR) has been developed as a promising noninvasive imaging tool for evaluating cardiac function and tissue characteristics comprehensively, including myocardial edema and fibrosis [8,9]. With these features, we assumed that CMR might also have potential in quantitatively assessing myocadiac injury for EHS patients and aimed to investigate this in this study.Materials and Methods
The institutional ethics committee of the Hospital approved the protocol of this prospective study. Written informed consent was obtained from each participant. This prospective study enrolled 28 male with EHI and 18 age-matched male healthy controls (HC). All participants were scanned on a 3.0T MRI scanner (Discovery MR750; GE Healthcare) with an 8-channel cardiac coil employed. For cine imaging, a fast imaging employing steady-state acquisition sequence was applied for assessing volumetric and functional parameters of the left ventricle (LV). Saturation methods using an adaptive recovery times (SMART1) sequence was performed at pre- and post-contrast injection for assessing native T1 and extracellular volume (ECV) . A multi-echo fast spin echo-based sequence with 4 TEs of 10.9, 27.2, 43.5, 59.8 ms was applied for acquiring T2 mapping. A multi-echo gradient echo-based sequence with 8 echo times was implemented for T2* mapping acquisition. LGE images were acquired in long-axis and short-axis views with a myocardial delayed enhancement (MDE) sequence 10-15 mins after an intravenous bolus of 0.2 mmol/kg of gadolinium-based contrast agent (Gadopentetaten Dimeglumine Injection, Beilu Pharmaceutical, China). All CMR images were analyzed using CVI 42 version 5.11.2 (Canada) by one senior radiologist. LV geometry and functional parameters were automatically processed with manual adjustments. Global T1, ECV, T2, and T2* values were averaged over the whole LV myocardium short-axis slices. To evaluate the reliability of native T1, ECV, T2, and T2* measures, a separate observer evaluated the CMR data of 20 randomly selected participants. The corresponding inter-observer agreement between the two observers was analyzed accordingly. Statistical AnalysisAll statistical analyses were conducted using SPSS (Version 26.0; USA). Student’s t-tests or Wilcoxon’s rank-sum tests were used for comparing the differences of continuous variables between groups. Chi-square tests or Fisher’s exact tests were used for comparing categorical variables, if possible. Comparisons among HC and two subgroups of patients were performed using one-way analysis of variance (ANOVA) analyses of variance with Bonferroni correction for post hoc comparisons (for normal distribution) or Kruskal-Wallis tests for post hoc pairwise comparisons (for non-normal distribution) as appropriate. Inter-observer agreement was tested by the intraclass correlation coefficient (ICC) analysis. A paired t-test was used to compare the three-month follow-up and baseline CMR data. A p value of less than 0.05 was considered statistically significant.Results
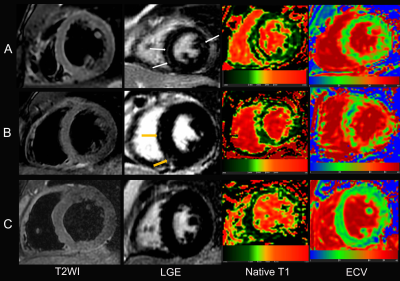
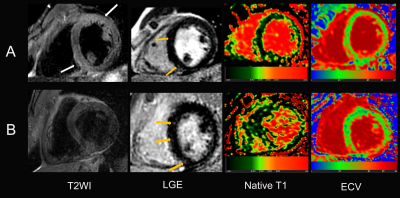
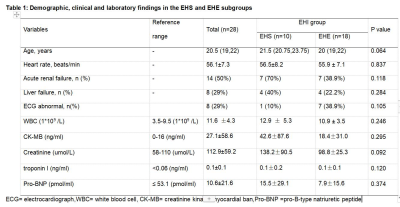
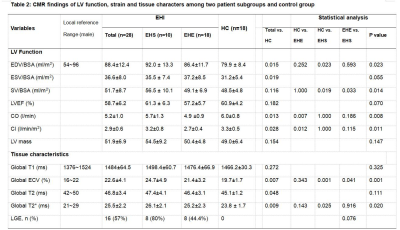
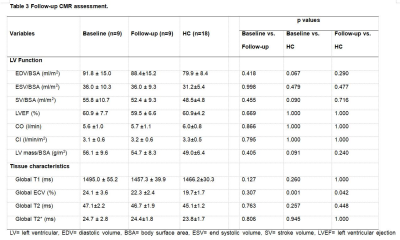
Table 1 shows the demographic and clinical features of the 46 subjects included. Table 2 shows the LV geometry, function and strain among the two patient subgroups and HC group.Compared to the HC group, EHI patients showed increased global ECV, T2 and T2* values. Among 28 EHI patients, 16 were found to have LGE in LV, located at the basal and mid segments (Figure 1). Eight patients had LGE at baseline and remained unchanged in follow-up LGE CMR (Figures 2). Table 3 shows there were no significant differences in all the parameters between baseline and follow-up, except for ECV. ECV in 9 EHI patients was significantly higher at follow-up than that of the HC group. Good interobserver agreement of CMR parameter measures, i.e., T1, ECV, T2, and T2*, were confirmed with high ICC values of 0.779, 0.882, 0.952, and 0.767, respectively.Discussion
To the best of our knowledge, this is the first CMR study to systematically assess LV morphology, function and myocardial tissue characterizations in EHS patients. As shown in this study, increased EDV, ESV, with decreased cardiac output and cardiac index were observed in EHI patients compared with age and sex matched HC. Quantitative myocardial tissue characterization showed myocardial edema and increased ECV indicating myocardial interstitial fibrosis in EHI patients with the highest value in the EHS subgroup. More than half of EHI patients were found to have LGE and the ventricular septum was the most involved location. More importantly, we found abnormally high ECV 3 months after the baseline CMR, indicating that myocardial injury of EHI patients was not recovered.Conclusions
With multi-parametric CMR, EHI patients demonstrated increased global ECV, T2, and persistent myocardial injury at 3-month follow-up after EHI episode. Therefore, multi-parametric CMR might be an effective method in evaluating myocardial injury in patients with EHI.Acknowledgements
NOReferences
1. Burkart KG, Brauer M, Aravkin AY, et al. Estimating the cause-specific relative risks of non-optimal temperature on daily mortality: a two-part modelling approach applied to the global burden of disease study. Lancet 2021;398:685-97.
2. Alele FO, Malau-Aduli BS, Malau-Aduli A, J Crowe M. Epidemiology of exertional heat illness in the military: a systematic review of observational studies. Int J Environ Res Public Health 2020;17.
3. Asmara I. Diagnosis and management of heatstroke. Acta Med Indones 2020;52:90-7.
4. Epstein Y, Yanovich R. Heatstroke. N Engl J Med 2019;380:2449-59.
5. Leon LR, Bouchama A. Heat stroke. Compr Physiol 2015;5:611-47.
6. Zhong L, Ji J, Wang C, Liu Z. Clinical characteristics and risk factors of male exertional heatstroke in patients with myocardial injury: an over 10-year retrospective cohort study. Int J Hyperthermia 2021;38:970-5.
7. Wallace RF, Kriebel D, Punnett L, Wegman DH, Amoroso PJ. Prior heat illness hospitalization and risk of early death. Environ Res 2007;104:290-5.
8. Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol 2018;72:3158-76.
9. Leiner T, Bogaert J, Friedrich MG, et al. SCMR position paper (2020) on clinical indications for cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2020;22:76.
Figures