3992
The value of DWI and T2 mapping in evaluating lymphatic vascular invasion of rectal cancer1The First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Philips Healthcare,Beijing, Beijing, China
Synopsis
Keywords: Digestive, Cancer
Lymphatic vascular invasion(LVI)can help clinicians choose the best treatment strategy for patients. Pathological examination is the gold standard for the diagnosis of LVI in rectal cancer, but it is an invasive method. Multiparametric magnetic resonance imaging is valuable for the prediction of LVI in rectal cancer. In this study, we quantitatively evaluated the value of LVI in rectal cancer using T2 mapping and DWI sequences.Synopsis
Lymphatic vascular invasion(LVI)can help clinicians choose the best treatment strategy for patients. Pathological examination is the gold standard for the diagnosis of LVI in rectal cancer, but it is an invasive method. Multiparametric magnetic resonance imaging is valuable for the prediction of LVI in rectal cancer. In this study, we quantitatively evaluated the value of LVI in rectal cancer using T2 mapping and DWI sequences.Summary of Main Findings
This study found that T2 and ADC values have good value for predicting LVI, and the combination of the two parameters improves the diagnostic efficiency, which is worthy of further exploration.Introduction
Rectal cancer (RC) is the second most common cancer in the large intestine and among the deadliest cancer in humans. Its prevalence and the number of young patients diagnosed with RC have been increasing . LVI , a tumor invading adjacent lymphatic vessels and/or blood vessels, is considered a strong stage-independent prognostic factor in RC patients and is an independent predictor of survival in RC patients. Therefore, accurate preoperative assessment of the LVI of RC is of great value for clinical decision-making and improvement of patient prognosis.Methods
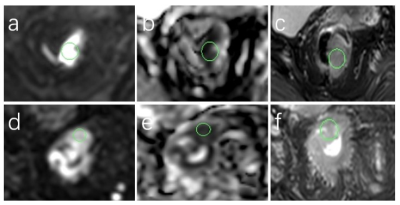
A total of 34 patients diagnosed with rectal cancer were recruited and scanned on a 3.0T MR Scanner (Ingenia CX, Philips Healthcare, Best, The Netherlands). These patients were divided into 2 groups based on whether tumour cells were observed in the lymphatic vessels and blood vessels in the vicinity of the collaterals on pathology: with vascular invasion (Group A, n=13) and without vascular invasion (Group B, n=21). Scan parameters are shown in Table 1. In the post-processing, the DWI images were fused onto the T2 mapping, and the ROIs were drawn on the slice with the largest lesion coverage (determined on DWI images) for each patient, avoiding the cystic degeneration and necrotic areas, mean area (32.4±11.2)mm2. (Figure 1). The Intraclass correlation efficient(ICC) analysis was performed to evaluate the agreement of the 2 observers' measurements.The ROIs were independently drawn by two radiologists, who recorded the measured T2 and ADC values as mean±SD. Independent Samples t-test or Mann-Whitney U test was used to evaluate the value of each parameter in predicting the disease between the two groups. The ROC curves were used to evaluate the predictive power of two parameter values.Results
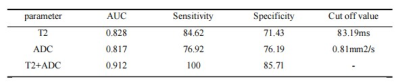
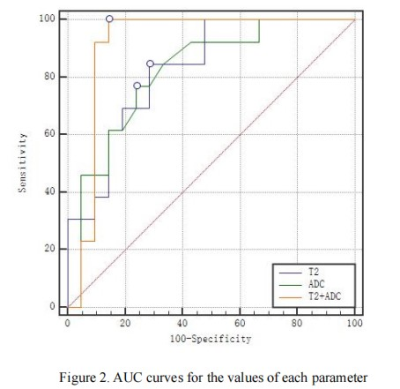
The measurement agreement between the two observers was good(ICC>0.75), as shown in Table 2. The ADC values and T2 values both showed significant differences (P<0.05)of the two groups of diseases, as shown in Table 3. The areas under the ROC curve of T2, ADC and T2-ADC value were 0.828,0.817 and 0.912 respectively. The sensitivity, specificity and threshold of T2 value in predicting vascular invasion were 84.62%, 71.43% and 83.19ms respectively, 76.92%, 76.19% and 0.81 mm2/ s for the ADC value,100% and 85.17% for the T2-ADC value, as shown in Table 4 and Figure 2.Discussion
T2 mapping and DWI sequences are both valuable in the quantitative assessment of LVI. The T2 and ADC measures reflect the water molecule content of tumour tissue cells and the dispersion of water molecules respectively. The two sequences are correlated to a certain extent. The combined diagnostic model has improved the efficacy of LVI diagnosis and has a good clinical application.Conclusion
This study shows that T2 mapping potentially provides a comparable metric to ADC in the prediction of LVI in rectal cancer, while the combination of the two measures merits improved predictive value in terms of larger AUC, higher sensitivity, and higher specificity.Acknowledgements
We thank the Philips Research team (Beijing, China) for guidance on this studyReferences
[1] Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209-249. doi:10.3322/caac.21660.
[2] Kim YI, Kim CW, Kim JH, et al. Clinical Implication of Perineural and Lymphovascular Invasion In Rectal CancerPatients Who Underwent Surgery After Preoperative Chemoradiotherapy. Dis Colon Rectum. 2021 Nov 24. doi: 10.1097/DCR.0000000000002219.
[3] Blumenthaler AN, Newhook TE, Ikoma N, et al. Concurrent lymphovascular and perineural invasion after preoperative therapy for gastric adenocarcinoma is associated with decreased survival. J Surg Oncol. 2021;123(4):911-922. doi:10.1002/jso.26367.
Figures
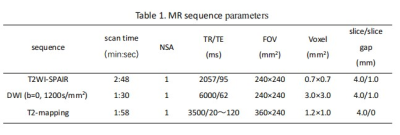
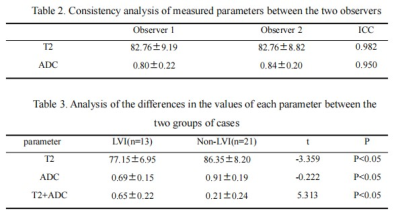
Table 2. Consistency analysis of measured parameters between the two observers
Table 3. Analysis of the differences in the values of each parameter between the two groups of cases