3985
Novel method for quantifying pancreatic exocrine function from Secretin-MRCP1Radiology, OHSU, Portland, OR, United States, 2OHSU, Portland, OR, United States, 3Medicine, OHSU, Portland, OR, United States
Synopsis
Keywords: Pancreas, Data Analysis
Chronic pancreatitis is a chronic fibro-inflammatory syndrome of the pancreas that often leads to exocrine pancreatic insufficiency EPI. Secretin MRCP provides an approach for quantifying function. Present interpretation of sMRCP lends itself to variability in interpretation . Further, previous approaches for quantitative assessment of sMRCP have been difficult to reproduce. We have developed a mathematical model for quantifying various features of dynamic sMRCP and have shown in a retrospective cohort, significant differences in one feature that correlates to delay of pancreatic production of fluid, to separate and correlate to ePFT and FE. 9Introduction
Chronic pancreatitis (CP) is a pathologic fibro-inflammatory syndrome of the pancreas characterized by pancreatic atrophy, fibrosis, pain syndromes, duct distortion and strictures, calcifications, pancreatic endocrine and exocrine dysfunction, and dysplasia. 1 Invasive imaging modalities such as endoscopic ultrasound (EUS) (with or without pancreatic function testing (PFT), and indirect PFT (e.g. Fecal elastase), and noninvasive (MRCP), have been used for decades . 1Secretin-enhanced MRCP (s-MRCP) introduces the use of synthetic secretin, a hormone which stimulates pancreatic duct epithelial cells to secrete bicarbonate. s-MRCP allows for exocrine pancreatic function . 2 This method however has subjectivity and relatively high variability amongst radiologists . 5 Although quantitative assessment of sMRCP has been previously been performed, 6–15 they have not demonstrated wide adaptability and reproducibility. Furthermore, their correlation with EUS PFT and FE have demonstrated mixed results.
Our goal in this work was to model the sMRCP data signal increases based on a logistic function that has been shown to approximate the increase and subsequent inhibition of the sphincter of Oddi during administration of secretin, . 17
Methods
Patient population: N=31 subjects with suspected EPI all of whom obtained standard of care sMRCP were enrolled in a retrospective IRB approved study comparing a novel quantitative assessment of sMRCP images and compared to reference standard fecal elastase (FE group (n=31)) or endoscopic pancreatic function test (ePFT group (n=8)).Pancreatic function testing: EPFT: Endoscopic pancreatic function testing was performed as previously described 18 following administration of 0.2mcg/kg of synthetic secretin with sampling of duodenal fluid taken from the 2nd portion of the duodenum performed with Peak bicarb concentration (highest of 4 collection or the collection at minute 45 post-secretin) > 80 IU/L reliably excludes a diagnosis of chronic pancreatitis. Fecal Elastase: FE1 was performed per standard of care as previously described 9 Values greater than 200 ug/g are considered normal without evidence of EPI. MRI MRCP: All patients were imaged at 1.5 or 3T using phased array body coils. Dynamic MRCP imaging was performed within one breath hold by using a single-shot HASTE fat saturated T2-weighted sequence (TE=600-700ms, TR=4500ms, FOV 300x380, slice thickness 46mm, flip 180). Slabs were taken dynamically prior to and immediately following intravenous administration of 0.2ug/kg secretin (ChiRhoStim) for a period of 20 second breath holds every minute for a period of 20 min.
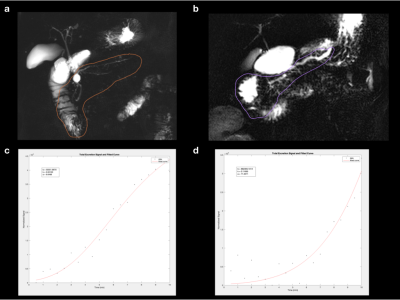
Image analysis: Images were analyzed by body trained radiologists with 2-20 years of training in MRCP of the pancreas and graded using established techniques with the ordinal scale of (0-3) based on extent of fluid within the duodenum.2 For quantitative analysis, a region of interest (ROI) was drawn around the pancreatic duct by a fourth year medical student with supervision from a body radiologist with 15 years of experience in body MRI and pancreatic imaging. The ROI included the entirety of the pancreatic duct and proximal duodenum (D1-D2). A normalized volume of water in the ROI was calculated by summing the signal values in each pixel in the ROI and dividing by the maximum signal in the image. The volume across all time points (20 points over 10 minutes) was fit using MATLAB using a logistic function with the equation
$$ V(t) = b* (1/1+e(-kt))a
where V is volume, t is time, b is a scaling value, k is a measurement of curve steepness, and a is a measure of delay in rise time. A logistic function was chosen to approximate the increase and subsequent inhibition of the sphincter of Oddi during administration of secretin, correlating with a sudden increase and plateau of pancreatic secretions.
Statistical Analysis: We compared clinical interpretations of sMRCP and fitted values from this equation in patients with normal ePFT to abnormal by using an unpaired, two-tailed t-test.
Results
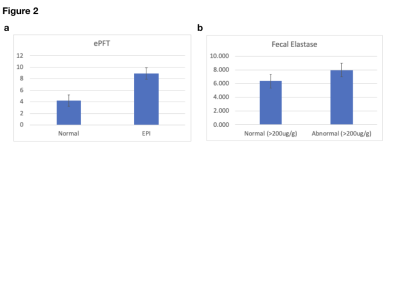
Figure 1a demonstrates an example of a patient with sequellae of CP as based on dilated branches, but no evidence of EPI based on standard radiologic interpretation of sMRCP data. Figure 1b also demonstrates an ROI on sMRCP of a patient with an abnormally dilated side branches and irregular duct. Of note, the subject in 1b demonstrated EPI based on FE and ePFT.Figure 2 demonstrates bar graphs from data analysis. Endoscopic PFT (n=8): 4/8 (50%) subjects were abnormal by ePFT. Although there was a statistically significant difference in the fitted value a (p<0.01) comparing both groups, no significance was achieved with standard clinical interpretations or other factors in the modeling.. Fecal elastase (FE) (N=31): 16/31 (52%) had pancreatic insufficiency by FE. There was also a statistically significant difference in a (p<0.05) comparing both groups. No significance was achieved with standard clinical interpretations or other factors in the modeling
Discussion
Our model quantifies the change in signal intensity as a function of a physiologically based logistic model based on endoscopic evaluation of the sphincter of Oddi. We hypothesize this to be more sensitive than volume and the fit value (a) in our model is representative of the delay seen in patients with EPI. This was borne out on this retrospective study. Further we feel that this approach lends itself to scalability and a semi-automated approach for quantifying EPI in patients in the futureAcknowledgements
No acknowledgement found.References
1. Conwell DL, Lee LS, Yadav D et al. American Pancreatic Association Practice Guidelines in Chronic Pancreatitis: evidence-based report on diagnostic guidelines. Pancreas 2014; 43, 1143-1162.
2. Swensson J, Zaheer A, Conwell D, Sandrasegaran K, Manfredi R, Tirkes T. Secretin-Enhanced MRCP: How and Why-AJR Expert Panel Narrative Review. AJR Am J Roentgenol 2021; 216, 1139-1149.
3. Tirkes T, Fogel EL, Sherman S et al. Detection of exocrine dysfunction by MRI in patients with early chronic pancreatitis. Abdom Radiol (NY) 2017; 42, 544-551.
4. Tirkes T, Yadav D, Conwell DL et al. Magnetic resonance imaging as a non-invasive method for the assessment of pancreatic fibrosis (MINIMAP): a comprehensive study design from the consortium for the study of chronic pancreatitis, diabetes, and pancreatic cancer. Abdom Radiol (NY) 2019; 44, 2809-2821.
5. Zuccaro P, Stevens T, Repas K et al. Magnetic resonance cholangiopancreatography reports in the evaluation of chronic pancreatitis: a need for quality improvement. Pancreatology 2009; 9, 764-769.
6. Bali MA, Sztantics A, Metens T et al. Quantification of pancreatic exocrine function with secretin-enhanced magnetic resonance cholangiopancreatography: normal values and short-term effects of pancreatic duct drainage procedures in chronic pancreatitis. Initial results. Eur Radiol 2005; 15, 2110-2121.
7. Bali MA, Golstein P, Devière J, Chatterjee N, Matos C. Evaluation of somatostatin inhibitory effect on pancreatic exocrine function using secretin-enhanced dynamic magnetic resonance cholangiopancreatography: a crossover, randomized, double blind, placebo-controlled study. Pancreas 2006; 32, 346-350.
8. Bali MA, Sontou R, Arvanitakis M, Metens T, Devière J, Matos C. Evaluation of the stimulating effect of a low dose of secretin compared to the standard dose on the exocrine pancreas with MRCP: preliminary results in normal subjects (MRCP quantification of secretin stimulation). Abdom Imaging 2007; 32, 743-748.
9. Bian Y, Wang L, Chen C et al. Quantification of pancreatic exocrine function of chronic pancreatitis with secretin-enhanced MRCP. World J Gastroenterol 2013; 19, 7177-7182.
10. Czakó L, Endes J, Takács T, Boda K, Lonovics J. Evaluation of pancreatic exocrine function by secretin-enhanced magnetic resonance cholangiopancreatography. Pancreas 2001; 23, 323-328.
11. Gillams A, Pereira S, Webster G, Lees W. Correlation of MRCP quantification (MRCPQ) with conventional non-invasive pancreatic exocrine function tests. Abdom Imaging 2008; 33, 469-473.
12. Gillams AR, Lees WR. Quantitative secretin MRCP (MRCPQ): results in 215 patients with known or suspected pancreatic pathology. Eur Radiol 2007; 17, 2984-2990.
13. Hafezi-Nejad N, Singh VK, Faghih M, Kamel IR, Zaheer A. Jejunal response to secretin is independent of the pancreatic response in secretin-enhanced magnetic resonance cholangiopancreatography. Eur J Radiol 2019; 112, 7-13.
14. Punwani S, Gillams AR, Lees WR. Non-invasive quantification of pancreatic exocrine function using secretin-stimulated MRCP. Eur Radiol 2003; 13, 273-276.
15. Schneider AR, Hammerstingl R, Heller M et al. Does secretin-stimulated MRCP predict exocrine pancreatic insufficiency?: A comparison with noninvasive exocrine pancreatic function tests. J Clin Gastroenterol 2006; 40, 851-855.
16. Albashir S, Bronner MP, Parsi MA, Walsh RM, Stevens T. Endoscopic ultrasound, secretin endoscopic pancreatic function test, and histology: correlation in chronic pancreatitis. Am J Gastroenterol 2010; 105, 2498-2503.
17. Geenen JE, Hogan WJ, Dodds WJ, Stewart ET, Arndorfer RC. Intraluminal pressure recording from the human sphincter of Oddi. Gastroenterology 1980; 78, 317-324.
18. Monachese M, Lee PJ, Harris K et al. EUS and secretin endoscopic pancreatic function test predict evolution to overt structural changes of chronic pancreatitis in patients with nondiagnostic baseline imaging. Endosc Ultrasound 2021; 10, 116-123.
Figures