3984
MR Elastography of the affected mesenteric fat in active Crohn’s Disease: a feasibility study1Radiology and Nuclear Medicine, AmsterdamUMC, location AMC, Amsterdam, Netherlands, 2Imaging and Biomarkers, Cancer Center Amsterdam, Amsterdam, Netherlands, 3Endocrinology, Metabolism, Amsterdam Gastroenterology, Amsterdam, Netherlands
Synopsis
Keywords: Digestive, Quantitative Imaging
Crohn’s Disease (CD) is a chronic inflammatory bowel disease. Mesentery of afflicted bowel loops often is involved. MR-Elastography allows assessment of its underlying mechanical properties and gives more insight in the role of the mesentery . Feasibility was first shown in 15 healthy volunteers. Seven patients with active CD (aCD) scheduled for surgical intervention underwent pre-operative MR-Elastography acquisition and histopathological analysis. Seven age- and sex matched volunteers were also scanned. Significantly higher shear wave speed, shear stiffness and phase angle were found in aCD patients, possibly related to increased fibrotic tissue in or inflammation of the mesentery.Introduction
Crohn’s Disease (CD) is a chronic inflammatory bowel disease and is often associated with the development of intestinal strictures and with increased and thickened mesenterial adipose tissue at disease locations (‘creeping fat’). Surgical resection of the affected bowel or stricturoplasty improves quality of life, however 50-70% of patients have recurrence and will require two or more surgical interventions.1 Recent literature suggests that bowel resection with extended mesenteric resection in patients with active Crohn’s Disease (aCD) of the ileocecal junction is associated with less postoperative recurrence.2-4 These findings make classification of mesenteric abnormalities highly relevant. This can be done at cross sectional imaging concerning creeping fat, but conventional anatomical imaging techniques fail to give more insight into the spectrum of involvement of the mesentery in the disease process, especially inflammation and fibrosis. A non-invasive method, such as MR-Elastography for determining the underlying mechanical properties of small-bowel mesentery could give more insight in the involvement of mesentery (inflammation, fibrosis) and the possible role in disease progression. The aim of this study was to show feasibility of MR-Elastograpy of the mesentery in patients with aCD.Methods
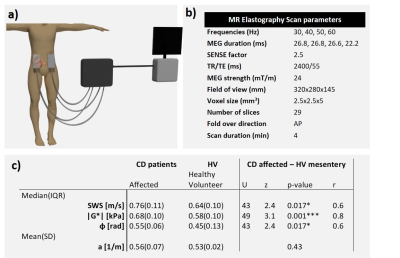
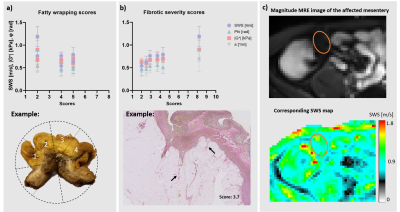
All scanning was done at 3.0T (Ingenia, Philips, Best, Netherlands). All subjects fasted four hours prior to scanning. Four compressed-air driven MRE-transducers were placed on the abdomen at the height of the ileocecal junction, two anterior and two posterior (see figure 1a). Elastography images were acquired with a multi-frequency free-breathing SE-EPI sequence at four frequencies (MREfreq=30,40,50,60Hz).5,7-8 Sequence parameters can be found in figure 1b, acquisition time was four minutes. Post-processing was accomplished using the (k)MDEV inversion algorithm resulting in shear-wave-speed (SWS), shear stiffness (|G*|), attenuation (a) and phase angle (φ) maps of the abdomen.5 Volumes-of-interest of the mesenteric fat at the height of the ileocecal junction were manually drawn on the mean magnitude images with guidance of T2-weighted images.Feasibility was shown in 15 healthy volunteers (9♀,34±10years), who underwent two consecutive MR-Elastography acquisitions to test within-session repeatability. Further, seven patients with aCD scheduled for surgical resection (2♀,40±16years) underwent one MR-Elastography acquisition. Seven age- and sex matched healthy volunteers underwent one MR-Elastography acquisition for comparison. Patients drank 1.5L of 2.5%-mannitol and healthy volunteers drank approximately 0.5L of water before their MR examination. Histopathology of the surgical specimen was possible in six (out of seven) patients who underwent surgical resection. Scores were given for fibrotic severity (based on percentage of fibrotic tissue in a histopathology segment of the mesentery using elastic-tissue-fibre (EvG) staining) and fatty wrapping around the small bowel-wall. Repeatability was assessed using Bland-Altman analysis. We tested for normality using the Shapiro–Wilk test. MR-Elastography parameters of SWS, |G*|, a and φ were analysed and compared between aCD patients and the age- and sex matched healthy volunteers using a paired t-test or Wilcoxon test, depending if the data was normally distributed. A significance level of 0.05 was used for all statistical tests.
Results
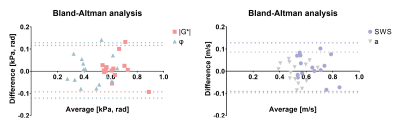
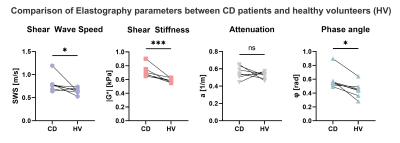
Healthy volunteer repeatability 95%-limits-of-agreement (LoA) were [-0.09, 0.13 m/s ], [-0.09, 0.12 kPa], [-0.10, 0.09 m/s] and [-0.12, 0.13 rad] for the SWS, |G*|, a and φ respectively, see figure 2. MR-Elastography parameters and scores for all patients can be found in figure 1c. Comparison of biomechanical properties with histopathology and fatty wrapping scores are depicted in figure 2 and 3. Shapiro-Wilk test for normality showed a normal distribution for attenuation only. Comparison with healthy volunteers showed no significant difference for the attenuation (mean a=[0.80±.0.21, 0.67±0.07 m/s], p=0.18), whilst the SWS, |G*| and φ did show significant differences (median SWS=[0.76(0.64-1.19), 0.64(0.53-0.74) kPa], |G*|=[0.68(0.65-0.90), 0.58(0.55-0.63) kPa], φ=[0.55(0.49-0.90), 0.45(0.28-0.64) rad], t=3, df=6, p=.02, p<.001, p=.02, respectively), see figure 4. In figure 5 an elastogram of a representative patient with aCD at the ileocecal junction is shown.Discussion
The repeatability of MR-Elastography of the mesentery at the level of the ileocecal junction was in line with previous published results of similar methods in other organs.6,7 LoA were lower for a than for φ, indicating that the kMDEV is a more precise post-processing algorithm for application in the mesentery. This is substantiated by the fact that the kMDEV takes the first derivative of the displacement data, as opposed to the second derivative in the MDEV, which can amplify noise.5 Comparison showed significant differences between patients and healthy volunteers for all elastography parameters, except for attenuation. An increase in SWS and |G*| suggests an increase in fibrotic tissue present in the mesentery in patients. This is also supported by the fibrotic severity score, which suggests a link between the SWS and the amount of fibrosis. The observed increase in φ in patients could be caused by an increase in vascularization and the presence of inflammation in the mesentery.8 The patient cohort is small, hampering strong conclusions, although the findings suggest a role of MR-Elastography in determining the severity of mesenteric inflammation and fibrosis in aCD patients.Conclusion
To conclude, our findings suggests that MR-Elastography may have the potential to measure the extent of inflammation and fibrosis of the affected mesentery in aCD. It could give more insight into disease progression and the role of the mesentery. Future research should look into the prognostic value of mesenteric MR-Elastography as a biomarker for CD recurrence after resection.Acknowledgements
No acknowledgement found.References
[1] Whelan G, et al. Recurrence after surgery in Crohn's disease. Relationship to location of disease (clinical pattern) and surgical indication. Gastroenterology. 1985;88:1826.
[2] Coffey CJ, Kiernan MG, Sahebally SM, Jarrar A, Burke JP, Kiely PA, et al. Inclusion of the Mesentery in Ileocolic Resection for Crohn's Disease is Associated With Reduced Surgical Recurrence. J Crohns Colitis. 2018;12(10):1139-50.
[3] Zhu Y, Qian W, Huang L, Xu Y, Guo Z, Cao L, et al. Role of Extended Mesenteric Excision in Postoperative Recurrence of Crohn's Colitis: A Single-Center Study. Clin Transl Gastroenterol. 2021;12(10):e00407.
[4] van der Does de Willebois EML, group Ss. Mesenteric SParIng versus extensive mesentereCtomY in primary ileocolic resection for ileocaecal Crohn's disease (SPICY): study protocol for randomized controlled trial. BJS Open. 2022;6(1).
[5] Meyer T, et al. Comparison of inversion methods in MR elastography: An open-access pipeline for processing multifrequency shear-wave data and demonstration in a phantom, human kidneys, and brain [published online ahead of print, 2022 Jun 12]. Magn Reson Med. 2022;10.1002/mrm.29320.
[6] Hsieh TJ, et al. Reliability of Gradient-Echo Magnetic Resonance Elastography of Lumbar Muscles: Phantom and Clinical Studies. Diagnostics (Basel). 2022;12(6):1385.
[7] Marticorena Garcia SR, et al. Tomoelastography for Measurement of Tumor Volume Related to Tissue Stiffness in Pancreatic Ductal Adenocarcinomas. Invest Radiol. 2020;55(12):769-774.
[8] 1. Shahryari M, Tzschatzsch H, Guo J, et al. Tomoelastography distinguishes noninvasively between benign and malignant liver lesions. Cancer Res. 2019;79(22):5704-5710. doi:10.1158/0008-5472.CAN-19-2150
Figures