3834
Ventricular flow analysis and its Association with cadiac function and structure of hypertrophic cardiomyopathy: 4D flow CMR study1The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China, 2MR Scientific Marketing, Siemens Healthineers Ltd., Guangzhou, China, 3Siemens Medical Solutions USA, Inc. Customer Solutions Group,Siemens Healthineers, MR Scientific Marketing, Siemens Healthineers Ltd., Chicago, IL, United States
Synopsis
Keywords: Cardiomyopathy, Cardiomyopathy, 4D flow
This study aimed to investigate the potential of ventricular flow parameters derived from four‑dimensional (4D) flow cardiovascular magnetic resonance (CMR) to accurately support assessment of hypertrophic cardiomyopathy (HCM). Our results show that reduced left ventricular (LV) residual volume was associated with LV dysfunction. Higher LV retained inflow and lower delayed ejection inflow were observed in obstructive HCM patients. Flow components and kinetic energy correlated significantly with LV functional and remodelling CMR parameters. These findings suggest that 4D flow CMR may be potential method to explain the relationship between hemodynamic and pathophysiological changes in HCM.Background
Four‑dimensional (4D) flow cardiovascular magnetic resonance (CMR) allows quantification of blood flow of the whole heart by flow components and kinetic energy (KE) analyses. However, the value of 4D flow parameters in hypertrophic cardiomyopathy (HCM) remains unclear. Current study aimed to investigate associations of 4D flow parameters with functional and remodelling parameters of left ventricular (LV) and compare 4D flow CMR parameters in obstructive HCM (oHCM) and non-obstructive HCM (noHCM).Methods
HCM patients were prospectively evaluated between 2020 and 2022. All underwent routine and 4D flow CMR on a 3.0-T MAGNETOM Trio MR scanner (Siemens Healthineers, Erlangen, Germany). The cardiac function and feature tracking (FT) of the LV over the whole cardiac cycle were conducted. Four flow components were analyzed: direct flow, retained inflow, delayed ejection flow and residual volume. Additionally, three phasic KE parameters normalized to end‑diastolic volume (KEiEDV), were analyzed for LV: peak systolic, average systolic and peak E‑wave.Results
Twenty-two HCM patients were prospectively recruited. LV residual volume correlated positively with LV end‑systolic volume index (ESVI) (r=0.442, P = 0.039) and LV mass index (r=0.453, P = 0.034). Direct flow correlated negatively with LV end‑diastolic volume index (EDVI) ,ESVI and mass index (all p<0.05). Peak systolic KEiEDV correlated significantly positively with average systolic KEiEDV and mass index (both p<0.05). Average systolic KEiEDV correlated positively with LV EDVI, mass index and global circumflex strain (GRS) (all p<0.05). In comparisons of oHCM and noHCM, LV retained inflow (20.78±6.53% vs. 9.72±3.80%, P <0.001) in oHCM were higher than in noHCM. LV delayed ejection inflow (15.22±6.43% vs. 21.86±7.00%, P=0.031) in oHCM were lower than in noHCM. A lower percentage of LV residual volume was more likely to result in LV dysfunction (OR=1.205, p=0.035).Discussion
This study aimed to investigate the potential role of 4D flow CMR in reflect cardiac function and structure in HCM. We observed reduced LV residual volume was associated with LV dysfunction. Higher LV retained inflow and lower delayed ejection inflow were observed in oHCM patients. The difference in the proportion of flow components between obstructive and non-obstructive HCM indicated a hemodynamic difference between the two. oHCM seems to be more prone to blood flow retention. Both LV direct and residual flows exhibited significant correlations with LV functional parameters and mass index. Peak and average systolic KEiEDV correlated significantly positively with mass index. KE represents work performed by the LV, which can be segmented temporally into different phases of the cardiac cycle or more granularly into the different flow components at different times.1 Previous studies have shown that increased LV mass leads to increased myocardial stiffness, microvascular dysfunction leads to myocardial ischemia and myocardial fibrosis, and these pathological changes are the pathological basis of left ventricular remodelling.2 Therefore, LV work and systolic energy change may be important parameters of left ventricular remodeling in HCM. Average systolic KEiEDV correlated positively with GRS, which may reveal the relationship between systolic KE change and LV myocardial deformation.3Conclusion
Ventricular flow parameters derived from 4D flow CMR correlated significantly with LV functional and remodelling CMR parameters. This supports its utility as an imaging parameter for monitoring disease progression and therapeutic response in HCM.Acknowledgements
No acknowledgement found.References
1. Robinson JD, Rose MJ, Joh M, et al. 4-D flow magnetic-resonance-imaging-derived energetic biomarkers are abnormal in children with repaired tetralogy of Fallot and associated with disease severity. Pediatr Radiol. 2019;49(3):308-317.
2. Yang WI, Shim CY, Kim YJ, et al. Left atrial volume index: a predictor of adverse outcome in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr. 2009;22(12):1338-1343.2.
3. Pedrizzetti G, Claus P, Kilner PJ, Nagel E. Principles of cardiovascular magnetic resonance feature tracking and echocardiographic speckle tracking for informed clinical use. J Cardiovasc Magn Reson. 2016;18(1):51.3.
Figures
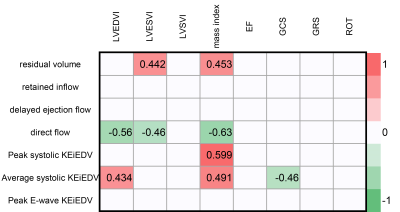
Figure 1 Significant correlation coefficient R of 4D flow parameters and LV function and structure parameters in hypertrophy cardiomyopathy
all p<0.05
KEiEDV, kinetic energy normalized to end‑diastolic volume; LVEDVI, left ventricular end‑diastolic volume index; LVESVI, left ventricular end‑systolic volume index; LVSVI, left ventricular stroke volume index; GRS, global circumflex strain; GRS, global radial strain; ROT, rotation.
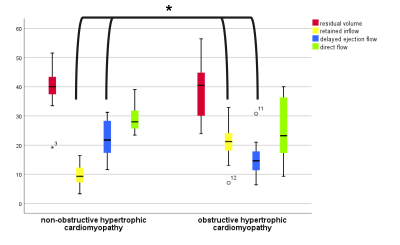
Figure 2 Comparisons of four flow components derived from 4D flow CMR between non-obstructive and obstructive hypertrophic cardiomyopathy.
*P < 0.05