3824
Patients with liver cirrhosis have more stagnant portal venous blood flow compared to non-cirrhotic subjects: analysis using 4D flow MRI1Radiology, Nagoya University Graduate School of Medicine, Nagoya, Japan, 2Fundamental Development for Advanced Low Invasive Diagnostic Imaging, Nagoya University Graduate School of Medicine, Nagoya, Japan, 3Radiological Technology, Nagoya Uviversity Hospital, Nagoya, Japan, 4RadiologicalTechnology, Nagoya Uviversity Hospital, Nagoya, Japan, 5Gastroenterology and Hepatology, Nagoya University Graduate School of Medicine, Nagoya, Japan, 6Transplantation Surgery, Nagoya Uviversity Hospital, Nagoya, Japan, 7Nagoya University Graduate School of Medicine, Nagoya, Japan
Synopsis
Keywords: Flow, Velocity & Flow
Although liver cirrhosis is an independent risk factor for portal vein thrombosis (PVT), the individual thrombotic risk assessment is complex. Recently, 4D flow MRI has begun to assess portal blood flow; however, there have been no reports of the use of RRT, an indicator of blood flow stagnation, in the portal system. RRT may be used to measure the risk of PVT in liver cirrhosis. In this study, we evaluated the mean RRT value of the main PV calculated with 4D flow MRI and found that the value was significantly higher in cirrhotic patients than in non-cirrhotic subjects.INTRODUCTION
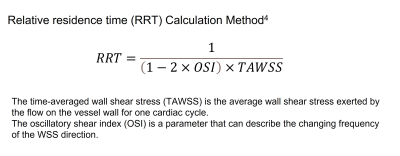
Portal vein thrombosis (PVT) is a severe complication in patients with cirrhosis and can exacerbate portal hypertension, an equally important complication (1). Although hypercoagulable conditions and infections are other causes of PVT, cirrhosis is an independent risk factor (1). Virchow’s triad of hypercoagulability, endothelial injury, and reduced blood flow is classically known for thrombus formation. However, the assessment of an individual patient’s thrombotic risk is complex.3D cine phase contrast MRI (4D flow MRI) is an imaging method that can display velocity vectors in three-dimensional space in a cardiac phase-resolved fashion (2). More recently, sporadic applications to the portal system have been reported (3). At the same time, primarily in the area of computational fluid dynamics (CFD), however, relative residence time (RRT, Fig.1) has been used to evaluate the stagnation of blood flow in the aorta (4). The usefulness of RRT has recently been reported in in-vivo cases using 4D flow MRI (5). If RRT is also applicable in the portal venous area, it may be used as a biomarker to measure the individual risk of PVT. To our knowledge, there have been no reports of RRT used in the portal venous region.
The purpose of this study was to evaluate RRT by portal blood flow analysis using 4D flow MRI and to assess the differences between non-cirrhotic subjects (non-cirrhotic group) and cirrhotic patients with portosystemic shunts (LC group).
METHODS
The institutional ethical committee approved the study, and informed consent for the 4D flow MRI was obtained from all patients. This study also conforms to the provisions of the Declaration of Helsinki.As the non-cirrhotic group, we included planned liver transplant donors who underwent preoperative non-contrast 4D flow MRI at our hospital between June 2020 and August 2022. In addition, as the LC group, we included cases with liver cirrhosis with portosystemic shunts and had contrast-enhanced 4D flow MRI from June 2021 to September 2022 at our hospital. Exclusion criteria were patients who refused the examination, patients for whom MRI was not indicated, and patients after surgery or intervention.
After >5 h of fasting, a 4D flow MRI was conducted using a 3T MR scanner (Prisma; Siemens AG Healthineers, Erlangen, Germany) with two 18-channel phased-array coils. In non-contrast cases, a coronal balanced steady-state free precession imaging was obtained for segmentation. In the LC group, a 3D coronal dynamic contrast‐enhanced MRI was obtained for segmentation, using 0.1 mmol/kg of gadobutrol (Gadovist; Bayer Yakuhin, Osaka, Japan) with an injection rate of 1 ml/s. Subsequently, a retrospective electrocardiogram‐gated 4D flow MRI with a respiratory navigator‐gating was conducted, including the upper abdomen, with the parameters listed in Table 1. Velocity encoding was calculated from portal flow velocity on 2D cine phase-contrast MRI for each patient prior to 4D flow MR imaging.
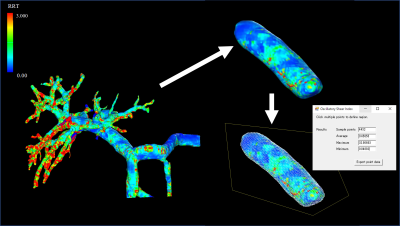
The 4D flow data were analyzed by one radiologist (11 years of experience in abdominal radiology and four years of experience in 4D flow MRI) and one radiological technologist (8 years of experience in 4D flow MRI). The 4D flow data set was post-processed using flow analysis software (iTFlow; Cardio Flow Design, Tokyo, Japan). The PV system was visualized by a 3D RRT map. Then, the main PV was extracted, and the spatial mean RRT value was measured (Fig. 2). RRT distribution was also visually evaluated.
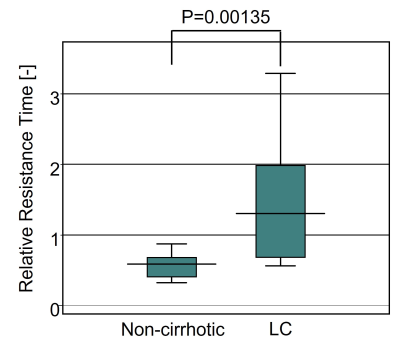
RRT values were shown as median and interquartile range. Comparison of RRT values between the two groups was performed with the Mann-Whitney U test using statistical software (StatFlex version 7; Artech Co., Osaka, Japan), and p<0.05 was considered significant.
RESULTS
Within the study period, 13 patients in the non-cirrhotic group (mean 45.0±10.1 years, range 27-56; M: F=8:5) and 13 patients in the LC group (mean 65.2±8.56 years, range 46-79; M: F=5:8) successfully underwent 4D flow MR imaging. No patients were excluded.The mean RRT value for the non-cirrhotic group was a median of 0.588 (interquartile range 0.410 to 0.681), and that for the LC group was a median of 1.304 (interquartile range 0.683 to 1.987). The LC group showed significantly higher values (p=0.00135, Fig. 3). No areas showed particularly high values by region.
DISCUSSION
The present study disclosed that the LC group had significantly higher mean RRT values than non-cirrhotic group, which is consistent with the fact that cirrhotic patients are more frequently associated with PVT. In this study, the mean RRT values in the LC group varied more than in the non-cirrhotic group. However, this may be because patients with various underlying diseases and liver functions coexisted in the LC group.Limitations of this study include the small number of cases in a single institution and the age difference between the two groups. Also, the non-cirrhotic group was imaged without contrast enhancement. The actual incidence of PVT was not evaluated because of a short evaluation period.
CONCLUSION
The patients with cirrhosis showed significantly higher RRT values than the non-cirrhotic subjects. RRT may be used as a biomarker to measure the individual risk of PVT.Acknowledgements
The authors thank Y. Sakurai, R.T. and S. Abe, R.T. for their technical assistance in image acquisition. This study was funded by JSPS KAKENHI (grant number JP19K17165).References
1. Intagliata NM, Caldwell SH, Tripodi A.Diagnosis, Development, and Treatment of Portal Vein Thrombosis in Patients With and Without Cirrhosis. Gastroenterology. 2019;156(6):1582-1599.e1.
2. Takehara Y. 4D Flow when and how? Radiol Med. 2020;125(9):838-850.
3. Hyodo R, Takehara Y, Naganawa S. 4D Flow MRI in the portal venous system: imaging and analysis methods, and clinical applications. Radiol Med. 2022;127(11):1181-1198.
4. Liu MY, Jiao Y, Liu J, et al. Hemodynamic Parameters Predict In-stent Thrombosis After Multibranched Endovascular Repair of Complex Abdominal Aortic Aneurysms: A Retrospective Study of Branched Stent-Graft Thrombosis. Front Cardiovasc Med. 2021;23;8:654412.
5. Trenti C, Ziegler M, Bjarnegård N, et al. Wall shear stress and relative residence time as potential risk factors for abdominal aortic aneurysms in males: a 4D flow cardiovascular magnetic resonance case-control study. J Cardiovasc Magn Reson. 2022;18;24(1):18.