3821
Quantitative characterization of hemodynamic parameters in pediatric patients with connective tissue disorders1Department of Medical Imaging, Ann & Robert H Lurie Children's Hospital, Chicago, IL, United States, 2Department of Radiology, Northwestern University, Chicago, IL, United States, 3Department of Cardiology, Ann & Robert H Lurie Children's Hospital, Chicago, IL, United States
Synopsis
Keywords: Flow, Cardiovascular, Marfan Syndrome, Loeys-Dietz Syndrome, Vascular Ehlers-Danlos syndrome
Quantitative overview of 4D flow derived aortic hemodynamic parameters such as kinetic energy, peak velocity, and pulse wave velocity in a cohort of pediatric patients with connective tissue disorders such as Marfan Syndrome (MFS), Loeys-Dietz Syndrome (LDS), and Vascular Ehlers-Danlos Syndrome (EDS), using a fully automated pipeline. A statistically significant trend of increased pulse wave velocity - an important measure of vessel stiffness, with increasing age was observed for this cohort. No association was found between PWV and all mean aortic diameters when controlled for age.Introduction
Patients with connective tissue disorders such as Marfan Syndrome (MFS), Loeys-Dietz Syndrome (LDS), and Ehlers-Danlos syndrome (EDS) show clinical overlap in cardiovascular manifestations1 such as aortic dilatation, aneurysms, and dissections. While the degree of severity varies, it is more pronounced for patients with LDS. Prior 4D flow MRI studies2-3 have demonstrated abnormal flow patterns in these patients which may lead to progressive aortic dilation and contribute further to adverse events. Hemodynamic parameters such as peak velocity and kinetic energy are of clinical interest for these patients, as their elevation is generally associated with higher risk of aortopathy. Additionally, pulse wave velocity (PWV), a surrogate measure of aortic wall stiffness that can be quantified from 4D flow MRI4 provides unique insights regarding both the innate tissue characteristics in these diseases and the development and progression of aortopathy. In this study, we report quantitative measurements of key aortic hemodynamic parameters using cardiovascular MRI including 4D flow in pediatric patients with connective tissue disorders.Methods
Forty-seven MFS, seven LDS, and two vascular EDS patients underwent clinically-indicated cardiac MRI including 4D flow. Patients with history of surgical intervention were noted from chart review. Imaging was performed at 1.5T and included either noncontrast or contrast-enhanced MRA and 4D flow with full 3D thoracic aorta coverage, sagittal oblique, and retrospective or prospective cardiac gating. The imaging parameters are as follows: FOV: 380-250 X 304-200 mm3, venc: 150-300 cm/s, temporal resolution: 38.0 – 39.9 ms, TR: 4.8-5 ms, TE 2.20-2.43 ms, flip angle: 8-25◦, free breathing with respiratory navigator. Using an in-house deep-learning pipeline, each 4D flow dataset was preprocessed for offset errors, noise-masking, and antialiasing, and followed by 3D aorta segmentation5,6. From the aortic segmentation, automated creation and placement of aortic centerline was performed using a modified 3D thinning algorithm. Along the centerline, two orthogonal 2D planes were placed around the branches of the innominate and subclavian arteries to subdivide the aorta in three regions of interest (ROI): ascending aorta (AAo), aortic arch (Arch), and descending aorta (DAo). Voxelwise hemodynamic 4D flow parameters like mean kinetic energy (KE) and peak velocity (Vmax) were then quantified for each aortic segment. Additionally, aortic diameters in each section were quantified by 3D geometric analysis of the aortic segmentation7. Diameters were calculated by automated method and differ from standard clinical measurements. Finally, global aortic PWV was quantified by a cross-correlation method applied to through-plane flow in a series of 2D analysis planes placed every 4mm along the centerline8. Correlations of PWV with age and aortic diameters were tested (Pearson coefficient), both for the patient cohort as a whole and for subcohort groupings of MFS patients and LDS patients each with no surgical intervention. ANCOVA analysis to test for baseline differences of MFS and LDS patients controlling for age was performed. A p-value <0.05 was considered as statistically significant for all statistical tests.Results
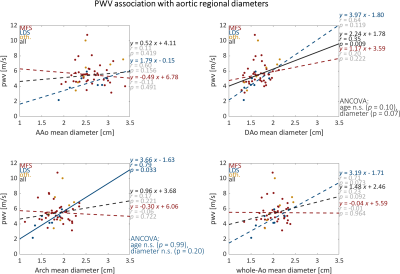
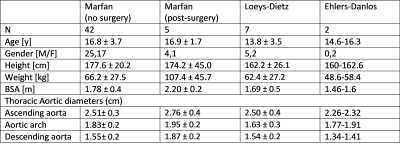
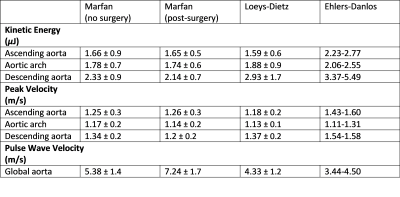
A total of 56 patients were included, with an age range of 4.1y to 22.6y (16.4y ± 3.7y; 34 males). Other patient characteristics are summarized in Table 1. Hemodynamic parameters for the three aortic segments are noted in Table 2. As shown in Fig. 1, there was a significant relationship between increased pulse wave velocity with increasing age (0.13 m/s/y, p=0.009) in the cohort of all subjects. PWV in the subgroups of LDS and MFS patients without surgery increased with age, but these trends were not statistically significant. Coefficients from ANCOVA analysis of PWV values in the combined subgroups using age as a covariate showed higher PWV in MFS patients than in LDS patients, but the effect was not found to be statistically significant (p=0.19). The correlation of PWV with all aortic mean diameters were not statistically significant except in the following cases: (1) PWV and arch mean diameter in LDS (p=0.03) and (2) PWV and DAo mean diameter in all subjects (p=0.009) (Fig. 2). Secondary analyses with ANCOVA using age as a covariate was performed and showed the effect was not statistically significant.Discussion
Establishment of baseline hemodynamic parameters in patients with connective tissue disorders is important, as they can differ greatly from the population at large. Trends of increasing pulse wave velocity with increasing age was observed in this cohort of pediatric patients with connective tissue disorder disease, and similar trends have been observed in healthy subjects and adult patients with valve disease9.Conclusion
We present a quantitative overview of hemodynamic metrics, such as Vmax, KE and PWV, in pediatric patients with connective tissue disorders. This overview gives a preliminary characterization of the ‘hemodynamic fingerprint’ for such patients. Further investigation with expanded subgroup (MFS, LDS) cohort sizes reference control groups of healthy subjects will help to establish normative ranges of these parameters in pediatric connective tissue disorder patients.Acknowledgements
No acknowledgement found.References
1. Meester JAN, Verstraeten A, Schepers D, Alaerts M, Van Laer L, Loeys BL. Differences in manifestations of Marfan syndrome, Ehlers-Danlos syndrome, and Loeys-Dietz syndrome. Ann Cardiothorac Surg. 2017 Nov;6(6):582-594.
2. van der Palen RL, Barker AJ, Bollache E, Garcia J, Rose MJ, van Ooij P, Young LT, Roest AA, Markl M, Robinson JD, Rigsby CK. Altered aortic 3D hemodynamics and geometry in pediatric Marfan syndrome patients. J Cardiovasc Magn Reson. 2017 Mar 17;19(1):30.
3. A Ruiz Munoz, A Guala, JF Rodriguez-Palomares, L Dux-Santoy, L Servato, A Lopez-Sainz, L La Mura, T Gonzalez-Alujas, L Galian-Gay, L Gutierrez, K Johnson, O Wieben, I Ferreira, A Evangelista, G Teixido-Tura, Aortic rotational flow patterns and stiffness by 4D flow CMR in patients with Loeys-Dietz syndrome compared to healthy volunteers and patients with Marfan syndrome, European Heart Journal - Cardiovascular Imaging, Volume 22, Issue Supplement_2, June 2021.
4. Markl M, Wallis W, Brendecke S, Simon J, Frydrychowicz A, Harloff A. Estimation of global aortic pulse wave velocity by flow-sensitive 4D MRI: Global Aortic Pulse Wave Velocity. Magn Reson Med. 2010 Jun;63(6):1575–82.
5. Berhane H, Scott M, Elbaz M, Jarvis K, McCarthy P, Carr J, et al. Fully automated 3D aortic segmentation of 4D flow MRI for hemodynamic analysis using deep learning. Magn Reson Med. 2020 Oct;84(4):2204–18.
6. Berhane H, Scott MB, Barker AJ, McCarthy P, Avery R, Allen B, et al. Deep learning–based velocity antialiasing of 4D‐flow MRI. Magnetic Resonance in Med. 2022 Jul;88(1):449–63.
7. Scott MB, Huh H, van Ooij P, Chen V, Herrera B, Elbaz M, et al. Impact of age, sex, and global function on normal aortic hemodynamics. Magn Reson Med. 2020 Oct;84(4):2088–102.
8. Jarvis K, Soulat G, Scott M, Vali A, Pathrose A, Syed AA, et al. Investigation of Aortic Wall Thickness, Stiffness and Flow Reversal in Patients With Cryptogenic Stroke: A 4D Flow MRI Study. J Magn Reson Imaging. 2020 Aug 31;53(3):942–52.
9. Johnson, E.M., Scott, M.B., Jarvis, K., Allen, B., Carr, J., Malaisrie, S.C., McCarthy, P., Mehta, C., Fedak, P.W., Barker, A.J. and Markl, M. (2022), Global Aortic Pulse Wave Velocity is Unchanged in Bicuspid Aortopathy With Normal Valve Function but Elevated in Patients With Aortic Valve Stenosis: Insights From a 4D Flow MRI Study of 597 Subjects. J Magn Reson Imaging
Figures