3819
Evaluation of pulmonary artery hemodynamic changes in COPD patients with different emphysema volume by using 4D-Flow MRI1Radiology, Tianjin Chest Hospital, Tianjin, China, 2Philips Healthcare, Beijing, China
Synopsis
Keywords: Flow, Blood, hemodynamic
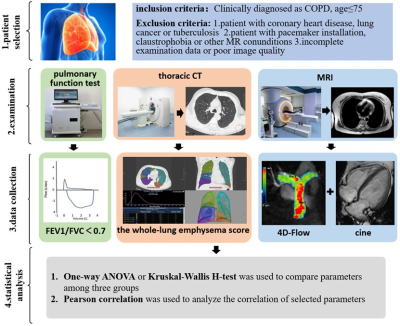
Few studies quantitatively evaluate pulmonary artery hemodynamic changes caused by emphysema. 34 COPD patients were divided into two groups according to emphysema volume and 12 healthy volunteers were matched. Hemodynamic parameters were calculated by 4D-Flow MRI and right ventricular function indicators were evaluated for three groups. The right systolic pressure drop and RVEF were lower in moderate and severe emphysema group but the right EL was higher. The whole-lung emphysema score correlated negatively with RVEF and the right systolic pressure drop. 4D-Flow combined with cine image can comprehensively evaluate the pulmonary artery hemodynamics and right ventricular function of COPD patients.Introduction
Emphysema is a pathological stage of substantial destruction of lung tissue in chronic obstructive pulmonary disease (COPD) patients. Excessive volume of emphysema will cause hemodynamic changes of pulmonary artery and further lead to impairment of right ventricular systolic function[1]. Right cardiac catheterization is the gold standard for quantifying pulmonary hemodynamics but with the disadvantages of invasive and risk. Hence reliable alternatives are urgently needed. 4D-Flow is a new technology of magnetic resonance blood flow imaging that can visually display blood flow and calculate relevant hydrodynamic parameters[2, 3]. However, there were few studies to quantitatively evaluate pulmonary artery hemodynamic changes and right ventricular contractility impairment caused by different emphysema volumes. Therefore, our goal was to analyze the pulmonary artery hemodynamics and right ventricular function in different volume classifications of emphysema.Method
34 patients diagnosed with COPD and 12 healthy volunteers were prospectively enrolled. All subjects underwent pulmonary function test, thoracic CT (SOMATOM Force or SOMATOM Definition, Siemens Healthineers, Forchheim, Germany) and 3.0T cardiac magnetic resonance (Ingenia CX, Philips Healthcare, Best, the Netherlands) including cine images and 4D-Flow sequence. The volume of emphysema was evaluated by quantitative CT software (IntelliSpacePortal Version 9.0; Philips Healthcare, Best, the Netherlands) and the whole-lung emphysema score was calculated as the percentage of lung voxels with intensity less than -950 Hounsfeld units (HU) on inspiratory scans. The quantitative parameters of cardiac and pulmonary artery hemodynamics were post-processed on CVI42 platform (version 5.13; Circle Cardiovascular Imaging, Calgary, AB, Canada). The hemodynamic parameters such as peak flow velocity (Vmax), average flow velocity (Vavg) and flow volume were measured in the mid-main pulmonary artery (MPA), mid-right pulmonary artery (RPA), and mid-left pulmonary artery (LPA) by 4D-Flow analysis. Besides, systolic pressure drop (PD) and viscous energy loss (EL) were calculated along two standardized anatomic trajectories including MPA – RPA tract and MPA – LPA tract, which starting at a plan defined by the pulmonary valve and ending at the terminus of the right or left pulmonary trunk. The right ventricular ejection fraction (RVEF) was measured semi-automatically. All data were performed by SPSS software, version 27 (IBM, Armonk, New York) . One-way ANOVA or Kruskal-Wallis H-test was used to compare parameters among the three groups, bonferroni method was used to do post HocComparison. Pearson correlation was used to analyze the correlations between Whole-lung emphysema score and RVEF, pulmonary artery flow parameters. P<0.05 were considered statistical significance. Research profile map showed in Figure 1.Result
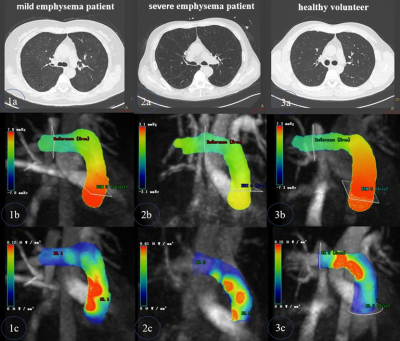
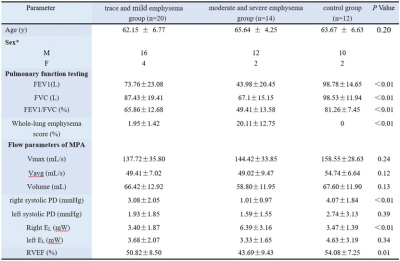
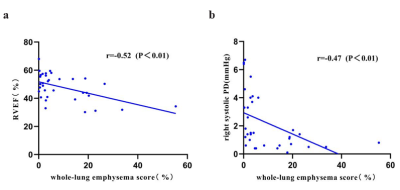
Participant characteristics and exam parameters were reported in Table 1. According to Fleischner Society classification system[4], COPD patients were divided into two groups, trace and mild emphysema group (n=20, 62.15 ± 6.77 years) which involved less than 5% of the lung zone,moderate and severe emphysema group (n=14, 65.64 ± 4.25 years) covered more than 5% of the lung zone. 12 healthy volunteers (63.67 ± 6.63 years) were included as control group. The right systolic pressure drop and RVEF of moderate and severe emphysema group was lower than that of trace and mild emphysema group and control group (1.01±0.97 vs 3.08±2.05 vs 4.07±1.84 mmHg, P<0.01), (43.69±9.43 vs.50.82±8.50 vs.54.08±7.25%, P=0.01). The right EL was higher than that of trace and mild emphysema group and control group (6.39±3.16 vs 3.40±1.87 vs 3.47±1.39 mW, P<0.01). (Figure2). The whole-lung emphysema score correlated negatively with RVEF and the right systolic pressure drop (r=-0.52, P<0.01), (r=-0.47, P<0.01).(Figure3).Discussion
Quantitative CT assessment of emphysema combined with cardiac MRI can analyze pulmonary artery hemodynamic changes and right ventricular function impairment in COPD patients due to increased emphysema volume[5]. In this study, it was recognized that continuous expansion of the area of alveolar residual air chamber would destroy capillaries in the alveolar interval, increasing the peripheral vascular resistance and the pressure at the distal pulmonary artery, which will further reduce the systolic pressure drop of pulmonary artery and then need more energy loss during the flow transmission. In addition, the lower pulmonary artery systolic pressure drop also increases the difficulty of right ventricular ejection, leading to the impairment of the right ventricular contractility. Because the right pulmonary artery is a natural continuation of the main pulmonary artery, this study showed a stronger association in MPA – RPA tract. Our limitation is that pulmonary artery pressure has not yet been measured, quantify pulmonary artery pressure will be needed in future investigation.Conclusion
Increased severity of emphysema tends to decrease the right systolic pressure drop, which lead more energy loss during the flow transmission and impairment of the right ventricular contractile function.Acknowledgements
NoneReferences
[1] Fei F, Koffman J, Zhang X, et al. Chronic Obstructive Pulmonary Disease Symptom Cluster Composition, Associated Factors, and Methodologies: A Systematic Review[J]. West J Nurs Res, 2022,44(4):395-415.
[2] Azarine A, Garcon P, Stansal A, et al. Four-dimensional Flow MRI: Principles and Cardiovascular Applications[J]. Radiographics, 2019,39(3):632-648.
[3] Gbinigie H, Coats L, Parikh J D, et al. A 4D flow cardiovascular magnetic resonance study of flow asymmetry and haemodynamic quantity correlations in the pulmonary artery[J]. Physiol Meas, 2021,42(2):25005.
[4] Lynch D A, Austin J H, Hogg J C, et al. CT-Definable Subtypes of Chronic Obstructive Pulmonary Disease: A Statement of the Fleischner Society[J]. Radiology, 2015,277(1):192-205.
[5] Oganesyan A, Hoffner-Heinike A, Barker A J, et al. Abnormal pulmonary flow is associated with impaired right ventricular coupling in patients with COPD[J]. Int J Cardiovasc Imaging, 2021,37(10):3039-3048.
Figures