3705
Feasibility of Deep Learning Reconstruction in Prostate Multiparametric MRI: a Preliminary Prospective Study1Radiology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy, Beijing, China, 2GE Healthcare, MR Research, Beijing, China
Synopsis
Keywords: Prostate, Machine Learning/Artificial Intelligence, Deep learning reconstruction
In this prospective study, feasibility of deep learning reconstruction (DLR) in axial FSE-T2WI and axial reduced-FOV DWI (FOCUS DWI) were evaluated compared with standard protocols. Fast protocol with DLR substantially reduced scanning time (axial FSE-T2WI: -32.1%; FOCUS-DWI: -36.8%). Fast FOCUS DWI with DLR showed the highest SNR and CNR for prostate PZ, TZ and lesion. Fast FSE-T2WI with DLR showed the highest SNR and CNR for prostate PZ and TZ. Moreover, fast FOCUS-DWI and FSE-T2WI with DLR demonstrated equivalent or better image quality than standard images. DLR may be useful in prostate multiparametric MRI protocol optimization and high-quality image acquisition.Purpose
Deep learning reconstruction has been reported as a new post-processing technique to reduce scanning time and improve image quality in several recent retrospective studies [1-4]. This study aimed to evaluate the value of deep learning reconstruction (DLR) in the prostate multiparametric MRI in a prospective clinical cohort.Methods
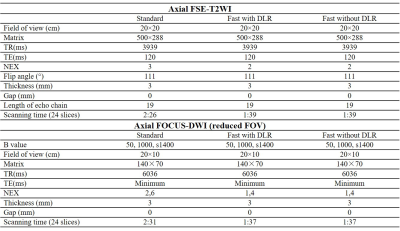
This is a prospective clinical cohort study approved by the institutional ethic board (NCC 3685). Patients suspected with prostate lesions were continuously enrolled into the scanning cohort. All MRI scannings were performed on GE 3.0T SIGNA Architect. All patients underwent a standard prostate mpMRI protocol (T1WI、axial/coronal/sagittal FSE-T2WI、DWI、reduced FOV DWI (FOCUS, b=50, 1000 and synthetic 1400) and dynamic enhanced scanning) and two study sequences (axial Fast FSE-T2WI with DLR and Fast FOCUS-DWI with DLR, b=50, 1000 and synthetic 1400), see Table 1. The original study images without DLR were also preserved. For qualitative image quality assessment, MRI scans were assessed with a five-point visual scoring system by two experienced radiologists independently. For FSE-T2WI, overall image quality, image artifacts, prostate capsule delineation and prostate lesion demonstration were evaluated. For FOCUS-DWI, overall image quality, image artifacts, prostate lesion demonstration were evaluated. Two radiologists independently assessed every prostate lesion’s Prostate Imaging-Reporting and Data System (PI-RADS) scores. The intraclass correlation coefficient (ICC) was used to compare the interreader agreement of qualitative scores and PI-RADS scores between two radiologists. For quantitative image quality assessment, the signal noise ratio (SNR) and the contrast noise ratio (CNR) of the prostate peripheral zone (PZ), transition zone (TZ) and prostate lesions were measured by one radiologist.Results
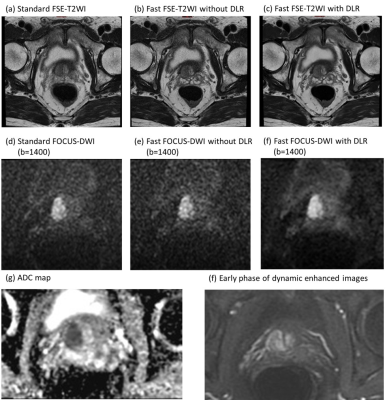
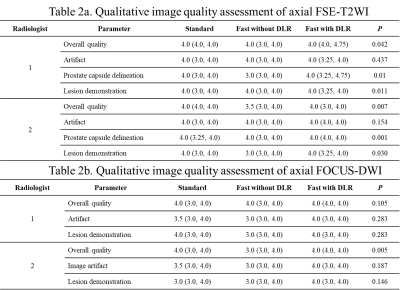
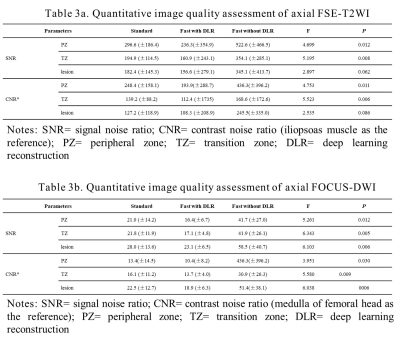
Finally, 26 patients were enrolled in this study with average age of 65.1±10.3 years old, and serum prostate specific antigen (PSA) level of 19.9±25.5ng/ml. For axial FSE-T2WI, fast protocol reduced 32.1% time (1min 39 seconds vs. 2min 26 seconds). For axial FOCUS-DWI, fast protocol reduced 36.8% time (1 min 37 seconds vs. 2 min 31 seconds). Two radiologists had good interreader agreement on the qualitative image quality evaluation (ICC: 0.70~0.85, with all p<0.05). Fast FSE-T2WI with DLR had the best overall image quality, prostate capsule delineation and prostate lesion demonstration among three sets of images. Image artifacts had no significant differences among three sets (see Table 2a). For FOCUS-DWI, three sets of images showed equivalent image quality (see Table 2b). A total of 29 prostate lesions (21 in peripheral zone and 8 in transition zone) were evaluated. Among them, 2 lesions were pathologically negative of prostate cancer and 12 lesions were pathologically proved clinical significant prostate cancer. Lesions’ ADC value had no significant differences among three sets of FOCUS-DWI images. Lesions’ PI-RADS score had no significant differences. For quantitative image quality assessment, fast axial FSE-T2WI with DLR had the highest SNR-PZ, SNR-TZ, CNR-PZ and CNR-TZ. SNR-lesion and CNR-lesion had no significant differences (see Table 3a). Fast axial FOCUS-DWI with DLR had the highest SNR-PZ, SNR-TZ, SNR-lesion, CNR-PZ, CNR-TZ and CNR-lesion (see Table 3b). Figure 1 showed an illustrative case with clinical significant prostate cancer.Conclusion
Fast scanning with deep learning reconstruction can substantially reduce scanning time, while acquire equivalent or better image quality than standard axial FSE-T2WI and reduced FOV DWI. Deep learning reconstruction may be useful in prostate multiparametric MRI protocol optimization and high-quality image acquisition.Acknowledgements
None.References
[1] Ueda T, Ohno Y, Yamamoto K, et al. Deep Learning Reconstruction of Diffusion-weighted MRI Improves Image Quality for Prostatic Imaging[J]. Radiology,2022,303(2):373-381. DOI: 10.1148/radiol.204097.
[2] Gassenmaier S, Afat S, Nickel MD, et al. Accelerated T2-Weighted TSE Imaging of the Prostate Using Deep Learning Image Reconstruction: A Prospective Comparison with Standard T2-Weighted TSE Imaging[J]. Cancers (Basel),2021,13(14):3593. DOI: 10.3390/cancers13143593.
[3] Gassenmaier S, Afat S, Nickel D, et al. Deep learning-accelerated T2-weighted imaging of the prostate: Reduction of acquisition time and improvement of image quality[J]. Eur J Radiol,2021,137:109600. DOI: 10.1016/j.ejrad.2021.109600.
[3] Kim EH, Choi MH, Lee YJ, Han D, Mostapha M, Nickel D. Deep learning-accelerated T2-weighted imaging of the prostate: Impact of further acceleration with lower spatial resolution on image quality[J]. Eur J Radiol,2021,145:110012. DOI: 10.1016/j.ejrad.2021.110012.
[4] Park JC, Park KJ, Park MY, et al. Fast T2-Weighted Imaging With Deep Learning-Based Reconstruction: Evaluation of Image Quality and Diagnostic Performance in Patients Undergoing Radical Prostatectomy[J]. J Magn Reson Imaging,2022,55(6):1735-1744. DOI: 10.1002/jmri.27992.
Figures