3651
Evaluation of PC-MRI Flow in Adults Using a Deep Learning-Based Reconstruction Trained on Pediatric Data
Matthew J. Middione1, Julio A. Oscanoa1,2, Xianglun Mao3, Christina R. Ruiz4, Michael Salerno1,4,5, Shreyas S. Vasanawala1, and Daniel B. Ennis1,5
1Department of Radiology, Stanford University, Stanford, CA, United States, 2Department of Bioengineering, Stanford University, Stanford, CA, United States, 3GE HealthCare, Menlo Park, CA, United States, 4Department of Medicine, Stanford University, Stanford, CA, United States, 5Cardiovascular Institute, Stanford University, Stanford, CA, United States
1Department of Radiology, Stanford University, Stanford, CA, United States, 2Department of Bioengineering, Stanford University, Stanford, CA, United States, 3GE HealthCare, Menlo Park, CA, United States, 4Department of Medicine, Stanford University, Stanford, CA, United States, 5Cardiovascular Institute, Stanford University, Stanford, CA, United States
Synopsis
Keywords: Flow, Machine Learning/Artificial Intelligence, Phase Contrast
We have previously trained a deep learning-based (DL) reconstruction for 2D PC-MRI using fully-sampled (n=194) raw k-space pediatric datasets. This DL-based reconstruction provided up to 9x undersampling with ≤5% error in accuracy and precision of peak velocity and total flow. Herein, we analyze this pediatric trained DL-based reconstruction in adult volunteers (n=3) and adult patients (n=8) and show that our DL-based reconstruction provides ~5% error in accuracy and precision of peak velocity and total flow for up to 7x undersampling.Introduction
2D Phase Contrast MRI (PC-MRI) provides time-resolved, quantitative measurements of blood flow throughout the cardiovascular system. 2D PC-MRI is used routinely in the clinic to quantify important parameters of cardiovascular health and disease, including peak velocity (cm/s) and total flow (mL). However, 2D PC-MRI acquisitions require breath holds to mitigate the impact of respiratory motion. Accurate and precise measurements of PC-MRI derived velocity and flow require spatiotemporal resolution that oftentimes necessitates upwards of 20 second breath holds, which is challenging for most patients.Previous work demonstrated a deep learning (DL)-based reconstruction capable of highly accelerated 2D PC-MRI datasets1. That work used fully-sampled raw k-space pediatric patient (n=194) datasets to train a DL-based reconstruction network. The DL reconstruction provided ≤5% error in both the accuracy and precision of pediatric patients’ peak velocity and total flow measurements when prospectively undersampled up to 9x.
The objective of this work was to evaluate the accuracy and precision of our 2D PC-MRI DL-based reconstruction (trained on pediatric data) applied to prospectively undersampled adult datasets.
Methods
The DL-based reconstruction network was constructed using fully-sampled, raw k-space 2D PC-MRI pediatric datasets (n=194), which were obtained with institutional IRB approval and patient consent. Imaging was performed using a 1.5T (n=23) or 3.0T (n=171) MR system (GE HealthCare, Waukesha, WI) and a vendor provided ECG-gated 2D PC-MRI sequence without parallel imaging (PI). The datasets were randomly divided into training (80%), validation (5%), and testing (15%) cohorts with a 155/10/29 split. Variable-density undersampling masks with 6-11x acceleration across the ky-t plane were randomly generated and applied on-the-fly to each dataset during training1.A prospective evaluation of the pediatric trained DL-based reconstruction was conducted in adult volunteers (n=3) and adult patients (n=8), both with IRB approval and consent, by acquiring 2D PC-MRI data in the ascending aorta (aAo) and main pulmonary artery (PA). A vendor provided ECG-gated spoiled gradient echo sequence with 2x PI was used for comparison. Data was also acquired using our custom ECG-gated spoiled gradient echo sequence with 6-8x variable-density undersampling applied across the ky-t. A repeated measurement was acquired for each sequence and imaged vessel in the adult volunteers to evaluate inter-scan variability. Aside from the fully-sampled free breathing scan, all subjects were asked to hold their breath at end expiration. Pulse sequence parameters and subject demographics are summarized in Table 1. The 2x PI datasets were reconstructed using the vendor provided reconstruction pipeline. The 6-8x undersampled images were reconstructed using the pediatric trained DL-based reconstruction.
All images were background phase corrected by masking regions of static tissue and fitting a second-degree polynomial to subtract background phase offsets from the vessel of interest2. ROIs were drawn in Horos3 and were loaded into Matlab along with the DICOMs to perform quantitative flow analysis. Measurements of peak velocity (mean value of the top 5% of all pixels contained in each vessel ROI) and total flow (mean vessel ROI velocity multiplied by the area of the vessel ROI integrated over the cardiac cycle) were compared. Inter-scan variability (root mean squared error, RMSE, and standard deviation) was compared for repeated scans with 2x PI and 6-8x DL for the adult volunteers. The measurement accuracy (RMSE) and precision (measured using the upper and lower 95%-confidence intervals, 95%-CIs) was evaluated across the adult volunteers and adult patient datasets using the 2x PI as the ground truth.
Results
A qualitative comparison of a representative adult patient (Figure 1) and adult volunteer (Figure 2) case demonstrates favorable agreement within the phase images for 2x PI and 7x DL. Inter-scan variability shows measurements of peak velocity and total flow are reproducible within 5% for 2x PI and 6-7x DL scans in adult volunteers (Table 2). A quantitative comparison of peak velocity and total flow measurements in the aAo and PA from the adult volunteers and adult patients show good agreement between 2x PI and 7x DL (Table 3). Specifically, 7x DL provides ~5% error in the accuracy and precision of measurements of peak velocity and total flow, relative to 2x PI.Discussion
This initial feasibility study shows that our DL-based reconstruction framework that was trained, tested, and evaluated using pediatric 2D PC-MRI datasets can provide ~5% error in the accuracy and precision of peak velocity and total flow measurements for 7x undersampling. This study shows that a lower undersampling rate (7x) is needed to maintain ≤5% accuracy and precision errors, relative to the pediatric study (9x). Nevertheless, these results indicate that our 2D PC-MRI sequence and DL-based reconstruction may have clinical utility in adult patient cohorts.The spatiotemporal resolution for this adult study closely matched that used in the pediatric study. Further investigation is needed to explore how higher or lower spatiotemporal resolution could impact the accuracy and precision of quantitative flow metrics. Future work could explore the use of transfer learning to train a new DL-based reconstruction network that incorporates adult data during training. This may enable higher undersampling rates in adult datasets.
Conclusion
Initial feasibility results show that a 7x prospectively undersampled 2D PC-MRI, reconstructed with a pediatric-trained DL-based reconstruction, provides ~5% error in the accuracy and precision of peak velocity and total flow measurements in adults.Acknowledgements
This project was supported, in part, by U01 EB029427 to SSV and support from GE HealthCare.References
- Oscanoa JA, Middione MJ, Syed AB, Sandino CM, Vasanawala SS, Ennis DB. Accelerated two‐dimensional phase‐contrast for cardiovascular MRI using deep learning‐based reconstruction with complex difference estimation. Magn Reson Med. 2022 Sep 12.
- Lankhaar JW, Hofman MB, Marcus JT, Zwanenburg JJ, Faes TJ, Vonk‐Noordegraaf A. Correction of phase offset errors in main pulmonary artery flow quantification. J Magn Reson Imag. 2005;22(1):73-9.
- Horos, v3.3.5; The Horos Project, LPGL license at Horosproject.org sponsored by Nible Co LLC d/b/a Purview in Annapolis, MD USA.
Figures
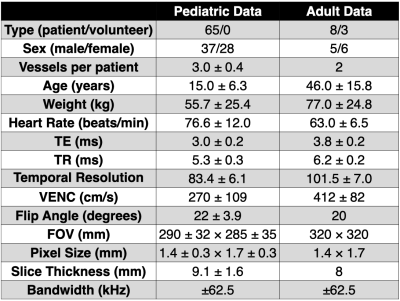
Table 1. Patient demographics and 2D PC-MRI imaging parameters from the pediatric datasets (n=194) used to train, evaluate, and test the DL-based network and the adult data (n=11) used to test the accuracy and precision of the pediatric DL-based reconstruction. The adult age, weight, and heart rate were significantly different than the pediatric data. The TE, TR, and temporal resolution were all increased for the adult data relative to the pediatric data, due to the increased FOV with the maintained in-plane spatial resolution, which necessitated an increased matrix size.
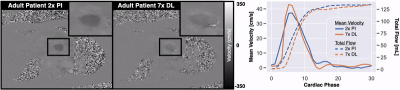
Figure 1. Qualitative results showing representative adult patient phase images acquired using 2x PI (left) and 7x undersampled, reconstructed with the DL-based reconstruction (right). Image quality is preserved for the DL-based reconstruction. Mean velocity and total flow curves show good agreement. The 7x DL peak velocity (106.4cm/s vs. 109.9cm/s) and total flow (135.1mL vs. 134.7mL) measurements were within 5% of the 2x PI scans.
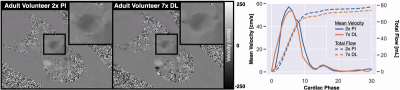
Figure 2. Qualitative results showing representative adult volunteer phase images acquired using 2x PI (left) and 7x undersampled, reconstructed with the DL-based reconstruction (right). Image quality is preserved for the DL-based reconstruction. Mean velocity and total flow curves show good agreement. The 7x DL peak velocity (73.2cm/s vs. 75.1cm/s) and total flow (78.0mL vs. 74.8mL) measurements were within 5% of the 2x PI scans.
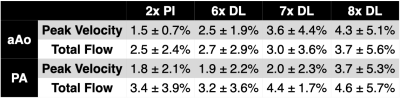
Table 2. Quantitative analysis of inter-scan variability from measurements in the ascending aorta and pulmonary artery of the healthy adult volunteers (n=3). A total of two scans were acquired per sequence, using both 2x PI and 7x DL and measurements of peak velocity and total flow were compared. All data is expressed as the root mean squared error (RMSE) ± standard deviation, calculated as a percent. 2x PI shows reduced inter-scan variability compared to 6-8x DL scans, but inter-scan variability is ≤5% for up to 7x DL.
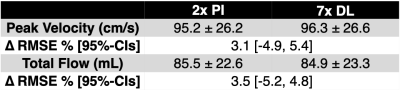
Table 3. Quantitative comparison of peak velocity and total flow in the aAo and PA from the adult volunteers and patients (n=11). Results are reported for 2x PI and 7x undersampled reconstructed with the DL-based reconstruction. Values for peak velocity and total flow are reported as the mean ± standard deviation in units of cm/s and mL, respectively. The difference between 2x PI and 7x DL is reported as the root mean squared error (RMSE) and the 95%-CIs, as a percentage relative to the 2x PI scan. The 7x DL scans show ~3% error in the accuracy (RMSE) and ~5% error in the precision (95%-CIs).
DOI: https://doi.org/10.58530/2023/3651