3552
Altered patterns of brain iron deposition in end-stage renal disease patients with depression
Yuan Li1, Yuhan Jiang1, Bingbing Gao1, Mingrui Qu1, Liangjie Lin2, Qingwei Song1, and Yanwei Miao1
1the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Philips Healthcare, Beijing, China
1the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Philips Healthcare, Beijing, China
Synopsis
Keywords: Gray Matter, Kidney
Both depression and end-stage renal disease (ESRD) may affect the pattern of iron deposition in human brain. This study aimed to quantify the changes of brain iron deposition in ESRD patients with and without depression using quantitative susceptibility mapping, and to further explore the effect of depression on iron deposition pattern in ESRD patients. Results showed that ESRD patients had increased brain iron deposition compared with heathy controls, especially in the left putamen and the right red nucleus, and ESRD patients with depression had less increase in iron deposition than those without depression.Summary of Main Findings
The magnetic susceptibility values (MSV) of gray matter nuclei in end-stage renal disease (ESRD) patients was measured by quantitative susceptibility mapping in this study with results showed that the MSV was increased, especially in the left putamen and the right red nucleus, in comparison to heathy controls; and those ESRD patients with depression had less increase than those without depression.Introduction
End-stage renal disease (ESRD) patients usually associated with impaired iron metabolism1, so that the clinical assessment of iron concentration does not reflect the patient's mental condition. There is currently a conflicting effect of iron on depression. Quantitative susceptibility mapping (QSM) has been shown to be the best method for detecting brain iron levels in vivo2. In this study, we aimed to quantitatively measure the magnetic sensitivity values (MSV) of gray matter nuclei in subjects using QSM and to determine the relationship between depression and ferrisis in ESRD patients.Methods
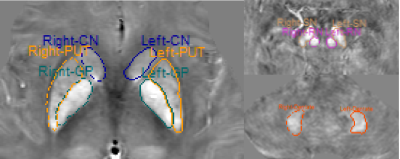
Thirty ESRD patients and 19 healthy controls (HCs, 8 females, 11 males, mean age: 56.42 ± 6.07 years) were prospectively recruited. According to the Hamilton Depression Scale scores (< 8 means without depression), the ESRD patients were further divided into ESRD with depression (D-ESRD) group (7 females, 9 males, mean age: 59.31 ± 6.74 years) and ESRD without depression (ND-ESRD) group (7 females, 7 males, mean age: 59.00 ± 10.38 years). Participants were scanned using a 3.0 T MR scanner (Ingenia CX, Philips Healthcare, Best, the Netherlands) with a 32-channel head coil to acquire the MR sequence of strategically acquired gradient echo (STAGE). Automatic measurements of MSV for deep gray matter nuclei on the QSM images reconstructed from the STAGE data was done using the signal processing in nuclear magnetic resonance (SPIN) software, and the regions of interest included bilateral caudate nucleus (CN), putamen (PUT), globus pallidus (GP), substantia nigra (SN), red nucleus (RN), and dentate nucleus (DN) (Figure 1). Clinical laboratory data of all subjects were collected. The MSV and clinical laboratory data were compared among the three groups using one-way analysis of variance, Bonferroni correction was applied to correct the multiple comparisons. Partial correlation analysis was used to assess correlations among the MSV and clinical and laboratory data in the D-ESRD group, with sex, age, education level as covariates.Results
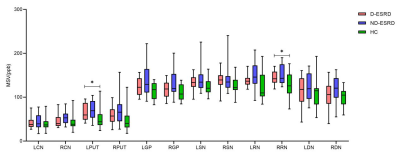
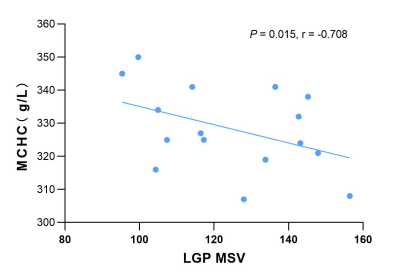
The MSVs of the ESRD group were increased in all gray matter nuclei in comparison with those of healthy controls. Significant differences of iron deposition were found in the left PUT and right RN between ESRD patients and HCs and the increase was more significant in patients of the ND-ESRD group (P = 0.021 and 0.048 after Bonferroni correction)(Figure 2) . The erythrocyte count, hemoglobin, red blood cell specific volume, mean corpuscular hemoglobin concentration and the estimated glomerular filtration rate (eGFR) were lower, but the red blood cell distribution width and the creatinine level were higher in the ESRD than in HC groups (after Bonferroni correction correction), but there were no significant difference between D-ESRD and ND-ESRD groups. The partial correlation analysis showed that the MSV of the left GP was positively correlated with mean corpuscular hemoglobin concentration (MCHC) (Figure 3) and negatively correlated with red blood cell distribution width (RDW) in D-ESRD group.Discussion
Due to impaired iron absorption, excessive loss, and iron supplementation during dialysis, clinical assessment of iron concentration in patients with ESRD does not reflect the real condition. In this study, QSM by the STAGE sequence was used to quantitatively measure MSV of gray matter nucleus, which represented iron deposition3, and further analyzed the effect of depression on brain iron deposition in ESRD patients. We found that MSV in left PUT and right RN of ESRD patients was significantly increased in comparison with HCs, and the increase were less in the D-ESRD group than in the ND-ESRD group. Further analysis showed that ND-ESRD group had a longer age on dialysis than patients with depression, which may be one of the reasons for the more pronounced increase in brain iron deposition. It has also been suggested that early iron supplementation can significantly improve postpartum depressive symptoms4. Therefore, further large-scale studies are needed to explore the relationship between depression and brain iron deposition. In addition, we found that MSV of left GP in D-ESRD group were negatively correlated with mean corpuscular hemoglobin concentration and positively correlated with red blood cell distribution width, indicating that the severity of anemia was positively correlated with brain iron deposition.Conclusion
Patients with ESRD had increased brain iron deposition, especially in the left putamen and the right red nucleus, and ESRD patients with depression show less increase in brain iron deposition than those without depression.Acknowledgements
No acknowledgement found.References
1. LIU Lei, ZHANG Mengjie, CHAI Chao, et al. The research progress of iron therapy in the treatment of anemia and brain iron deposition in patients with chronic kidney disease. Int J Med Radiol 2016 Sep; 39(5).
2. Haacke EM, Liu S, Buch S, et al. Quantitative susceptibility mapping: current status and future directions. Magn Reson Imaging. 2015 Jan;33(1):1-25.
3. HALLGREN B, SOURANDER P. The effect of age on the non-haemin iron in the human brain. J Neurochem. 1958 Oct;3(1):41-51.
4. Sheikh M, Hantoushzadeh S, Shariat M, et al. Retraction Note to: The efficacy of early iron supplementation on postpartum depression, a randomized double-blind placebo-controlled trial. Eur J Nutr. 2022 Dec;61(8):4239.
DOI: https://doi.org/10.58530/2023/3552