3543
MRI of Neuroinflammation in the Brain following Meth Addiction using Multiplied, Added, Subtracted and/or Divided (MASDIR) sequences.1Mātai Medical Research Institute, Gisborne, New Zealand, 2Faculty of Medical and Health Sciences & Centre for Brain Research, Auckland, New Zealand, 3Department of Neuroscience,, University of Otago, Dunedin, New Zealand, 4New Zealand P Pull, Tairāwhiti-Gisborne, New Zealand, 5Ngati Porou, Aotearoa, New Zealand, 6Tūranga Health, Tūranganui-a-kiwa, Gisborne, New Zealand, 7Ngāti Porou, Ngāti Kahungungu, Rongomaiwahine, Rongowhakaata; Tūranganui-a-Kiwa, Tairāwhiti, New Zealand, 8University of California San Diego, San Diego, CA, United States
Synopsis
Keywords: Neuroinflammation, Drugs, brain, methamphetamine, white matter hyper intensities
Keywords; Neuroinflammation, data acquisition and post processing, contrast mechanisms, white matter, drugs.
MR contrast can be enhanced by exploiting the concept of tissue property filters (TPFs) by designing Multiplied, Added, Subtracted, and/or Divided Inversion Recovery (MASDIR) sequences to amplify contrast produced by small changes in white matter T1. The Divided, Subtracted IR (dSIR) sequence provides very high contrast depiction of subtle white matter changes due to disease that are not identified with standard T2-FLAIR imaging. This was demonstrated in patients with a history of methamphetamine addiction. MASDIR sequences could revolutionize the way that neuroinflammation is imaged in clinical practice.
Purpose
Methamphetamine (meth) use is a pervasive problem with ~6% of New Zealanders having used the drug. This use is disproportionately higher among poor and disadvantaged people. A subset of meth users develop methamphetamine associated psychosis (MAP) which has a poorer prognosis and results in decreased cognitive function compared to the prognosis for patients with no psychosis (MNP).Changes to the brain associated with meth use include atrophy and white matter hyperintensities (WMH) that can be depicted and quantified with standard MRI sequences1,2. As with other diseases such as multiple sclerosis, meth use causes chronic neuroinflammation which may be difficult to detect with conventional MRI3.
Neuroinflammation encompasses a wide range of humoral and cellular responses ultimately aimed at control and repair. Different cell types and molecular mediators participate in a cascade of events in the brain enabling the central nervous system (CNS) to fight noxious events but can also result in lasting damage to the brain4. Depicting these changes with imaging is difficult but demonstrating subtle neuroinflammation could serve as a marker for recovery, as a predictor of the patient’s ability to abstain from use, and as an indicator for future psychosis.
The main pulse sequences used in clinical MRI diagnosis of WM disease are the T2-w spin echo (T2-wSE) and T2-FLAIR. We have developed a new framework for describing the contrast between different tissues on MRI which led to the implementation of Multiplication, Addition, Subtraction and Division of conventional Inversion Recovery (MASDIR) sequences5 (Figs. 1 and 2).
In the particular case of the divided Subtracted IR (dSIR) sequence, the contrast produced by an increase of T1 in the sensitive middle Domain (mD) of the sequence may be five or more times greater than that produced by a conventional IR sequence (Fig. 2C). We hypothesize that the dSIR sequence will be able to image areas of suspected neuroinflammation in the WM of meth users that are not seen with conventional state-of-the-art pulse sequences.
Methods
With ethical approval, four past meth users (2 males and 2 females 20-51-years-old) and four normal controls were scanned on a 3T MRI scanner (SIGNA Premier; General Electric Healthcare, Milwaukee, WI) with an AIR™ 48-channel head coil. Standard 2D FSE IR and 3D fast-SPGR IR (BRAVO) sequences were acquired with inversion times (TIs) chosen to produce dSIR images. A short TI was selected to null white matter (WM) and two increased TIs were used to provide contrast in narrow and wide middle Domains (mDs). An in-house built MATLAB code (MathWorks, Natick, WA) was used to produce dSIR images. T2-FLAIR images were acquired for comparison.Results
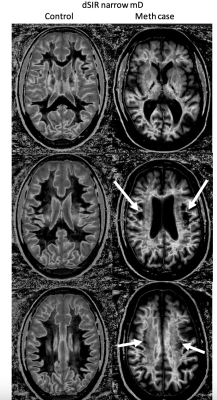
We show results from two male patients (49 and 50 y/o) both with 20+ years of meth use who were abstaining from use (for 120 and 80 days respectively) at the time of their respective MRI examinations.Fig. 3 shows 2D dSIR narrow and wide mD images acquired on a healthy control matched for age, gender, ethnicity, and socio-economic status with the 49 y/o volunteer. In the normal control, the dSIR images showed WM as low signal (dark, left column). In the meth patient, the dSIR narrow mD images showed extensive higher signal changes in WM with only small areas of healthy WM (right column). The dSIR images also showed high contrast and high spatial resolution boundaries between WM and grey matter (GM) which can be explained by the physics of IR imaging.
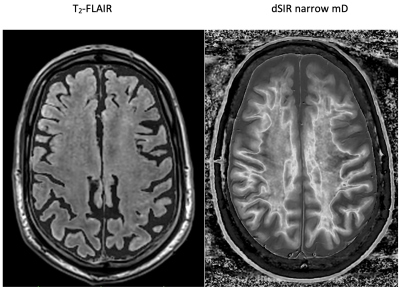
Fig. 4 shows T2-FLAIR and narrow mD dSIR images through the centrum semiovale in the same patient as in Fig. 3. Little or no abnormality is seen on T2-FLAIR image (left), but extensive abnormalities are seen on the narrow mD dSIR image (right). There are small areas of normal low signal (dark) WM on the dSIR image, but about 90% of the WM is higher signal and appears abnormal. High signal boundaries are again seen on the narrow mD dSIR image.
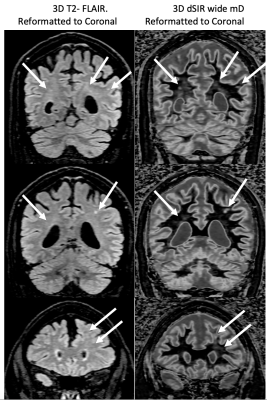
Fig. 5 shows coronal reformatted 3D T2-FLAIR and 3D wide mD dSIR images acquired on the 50 y/o volunteer after 80 days of abstinence. The T2-FLAIR and wide mD dSIR images show similar appearances of focal lesions (arrows). This highlights the importance of using a narrow mD with the dSIR sequence to show subtle abnormalities.
Discussion
We have shown that a precise understanding of MRI tissue contrast can provide a basis for developing sequences that are exquisitely sensitive to changes in WM T1. In meth users these sequences depicted WM changes that were not identified with standard T2-FLAIR images. This makes depiction of subtle changes in WM far easier. These changes may give a better understanding of the severity of disease processes and the prognosis with abstinence.Conclusion
The narrow mD dSIR sequence depicts widespread WM changes far better than the standard T2-FLAIR sequence. This framework could revolutionize the way that neuroinflammation is imaged with applications in post viral syndrome, substance abuse, brain injury and neurodegenerative disease. Importantly, these images can be obtained on any MRI scanner capable of performing standard IR FSE and gradient echo sequences, potentially making the approach readily available worldwide.Acknowledgements
We would like to acknowledge support from the Fred Lewis Enterprise Foundation, Wendy Nohi, and Kānoa – Regional Development Unit, New Zealand. We are also grateful for support from GE Healthcare and Mātai Ngā Māngai Māori, as well as our research participants.References
- Chang L, Alicata D, Ernst T, Volkow N. Structural and metabolic brain changes in the striatum associated with methamphetamine abuse. Addiction. 2007;102 (1):16–32
- Andres T, Ernst T, Oishi K, Greenstein D, Nakama H, Chang L. Brain Microstructure and Impulsivity Differ between Current and Past Methamphetamine Users. J Neuroimmune Pharmacol. 2019;11(3): 531–541. doi:10.1007/s11481-016-9675-8
- Piehl F. Current and emerging disease modulatory therapies and treatment targets for multiple sclerosis. J Intern Med. 2021;289(6):771–91
- Quarantelli M. MRI/MRS in neuroinflammation: methodology and applications. Clin Transl Imaging 2015;3:475–489
- Ma YJ, Moazamian D, Cornfeld DM, Condron P, Holdsworth SJ, Bydder M, Du J, Bydder GM. Improving the understanding and performance of clinical MRI using tissue property filters and the central contrast theorem, MASDIR pulse sequences and synergistic contrast MRI. Quant Imaging Med Surg.2022;12(9):4658-90
Figures