3535
Whole Brain MRI Reveals that Children with Acute Disseminated Encephalomyelitis have Enlarged Brain Ventricles at Disease Onset1Berlin Ultrahigh Field Facility, Max Delbruck Center, Berlin, Germany, 2Experimental and Clinical Research Center, Charité - Universitätsmedizin Berlin, Berlin, Germany, 3Division of Paediatric Neurology, Department of Paediatrics, Medical University of Innsbruck, Innsbruck, Austria, 4Department of Paediatric Neurology, Children's Hospital Datteln, Witten/Herdecke University, Datteln, Germany, 5Department of Neurology, Charité - Universitätsmedizin Berlin, Berlin, Germany
Synopsis
Keywords: Neuro, Neuroinflammation, acute disseminated encephalomyelitis
Pediatric patients with acute disseminated encephalomyelitis (ADEM) are at risk of long-term neurocognitive consequences. We investigated a multi-center cohort of ADEM patients with serial whole brain MRI, to distinguish transient reversible expansion of brain ventricle volume (BVV) from persistent changes. Using the automated brain segmentation tool SynthSeg, we observed that ADEM patients had significantly enlarged BVV relative to sex- and age-matched pediatric control subjects, already at the first clinical presentation, before any steroid treatment. Most ADEM patients developed even greater BVV expansion over the observation period. The majority of patients recovered, though some showed persistent BVV enlargement, suggesting brain atrophy.Introduction
Acute disseminated encephalomyelitis (ADEM) is an inflammatory disorder of the central nervous system, that can affect young children.1 Pediatric ADEM patients are at risk of long-term neuropsychiatric consequences.2 Previously we reported a profound enlargement of brain ventricle volume (BVV) in the experimental autoimmune encephalomyelitis (EAE) model of neuroinflammation, which normalized upon remission of clinical signs.3 We also reported that a majority of adult relapsing-remitting multiple sclerosis patients showed transient increases in BVV, and that patients with volatile BVV appeared to be at an earlier stage of their disease.3 This suggests that transient BVV changes may be a marker of inflammatory processes. In this study, we examine longitudinal whole brain MRI scans from a multi-center cohort of pediatric ADEM patients, to identify similar transient BVV changes, and to distinguish these from persistent BVV expansions that indicate irreversible brain atrophy.Methods
Whole brain MRI scans from pediatric patients with confirmed ADEM at disease onset (prior to steroid treatment) and follow-up scans were obtained from 35 pediatric neurology clinics in Germany, Austria, Italy, Switzerland and Canada: n=66; 34/66 female; mean age=6.54 years (range 0.66-19.6). This data was obtained from routine clinical practice; MRI scan parameters varied among centers, with variable timing of follow-up scans, according to the clinical needs of individual patients.3D whole brain MRI scans of healthy pediatric subjects were obtained from the National Institutes of Health (NIH) Pediatric MRI Data repository, Adolescent Brain Cognitive DevelopmentSM Study4 (1st cohort n=464, scanned at 1.5T; 2nd cohort n=652 subjects, scanned at 3.0T). A third cohort (n=122, scanned at 3.0T) was obtained from the open-source Pixar study.5 In total, we included n=1219 healthy controls, mean age=11.83 years (range 0.17-21.92).
Fully-automated brain segmentation was performed using SynthSeg.6,7 This was developed as a convolutional neural network-based brain segmentation tool, that is agnostic to MR contrast and scan resolution. SynthSeg was selected as the most appropriate tool, given the heterogeneous ADEM patient dataset. All patient scans were manually screened, and segmentations examined for quality control. Scans of all healthy controls were processed using the same version of SynthSeg; segmentations from 19 controls were excluded due to poor image quality. Data analysis was done using the statistical computing environment R v4.2.1.
Results
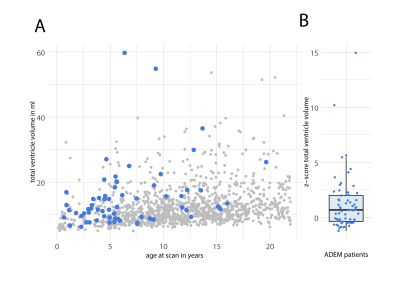
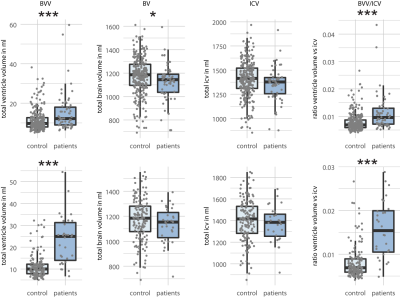
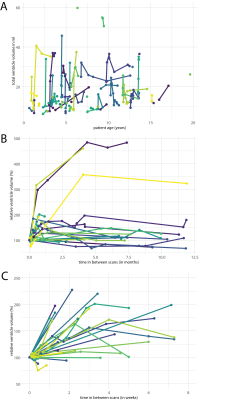
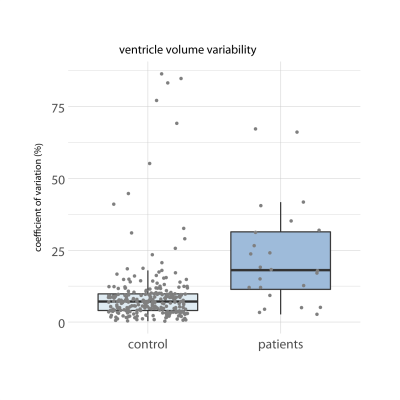
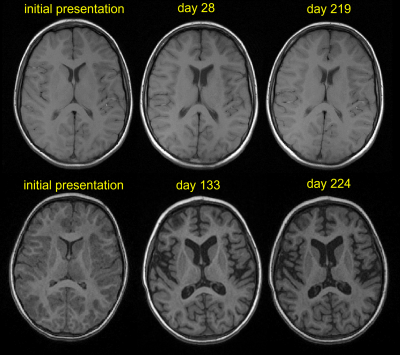
Upon initial clinical presentation, and prior to steroid treatment, ADEM patients showed enlarged BVV, compared to healthy controls (Fig.1A). Patient BVV Z-scores were calculated relative to 10 randomly sampled age-matched (±12 months) and sex-matched controls. Mean Z-scores from 10 iterations of random sampling of controls show a positive skew (Fig.1B). ADEM patients had significantly larger BVV and lower brain volume (BV) at initial presentation (Fig.2A). There was no significant difference in intracranial volume (ICV), and consequently a significant increase in the ratio of BVV:ICV. Most patients showed even further increases in BVV after initial presentation. The maximum BVV within 2 months from initial presentation (acute disease phase) is depicted in Fig.2B; the enlargement of BVV and increase in the BVV:ICV ratio was even more pronounced. Many patients showed even greater changes in BVV at later timepoints (Fig. 3A). This longitudinal plot showing changes in absolute BVV across the age range of the patient cohort. Substantial heterogeneity in BVV variability was observed in relative BVV values (compared to baseline) within the first year (Fig.3B) and first 2 months from initial presentation (Fig.3C). ADEM patients had a significantly greater coefficient of variation of BVV compared to healthy controls (calculated for cases with >2 scans) (Fig.4). The majority of ADEM patients recovered from the BVV increase, however 17/66 showed a persistent BVV increase of >5%, and 9/66 showed a persistent increase of >25%, relative to baseline. Representative MR images of a patient with a transient BVV increase that subsequently resolved are shown in Fig.5A. This patient recovered from clinical signs. Fig.5B shows a patient with a very large increase in BVV that failed to resolve, likely reflecting irreversible brain atrophy. This patient had a residual EDSS=1, and cognitive impairment at the time of the last scan (Fig.5B–right).Discussion
We report here that BVV in pediatric ADEM patients was enlarged relative to age- and sex-matched healthy controls, already at first clinical presentation. Importantly, the first MR scans in all patients were performed prior to administration of steroids, or any other disease modifying therapies. Thus, pseudoatrophy can be excluded. Most patients showed even greater increases in BVV during the course of the observation period. Nevertheless, the majority of patients recovered from this BVV expansion, suggesting that it was a consequence of processes associated with acute disease, rather than irreversible brain atrophy. However, some patients did show persistent BVV changes. Further analysis of how BVV changes relate to other clinical parameters is ongoing. Together with other clinical outcomes, MRI monitoring of BVV changes could be an important clinical biomarker to differentiate between transient and persistent changes, and support appropriate treatment decisions. Effective, easy to use tools for robust segmentation and analysis of brain MRI will be crucial for widespread application in routine clinical practice.Acknowledgements
No acknowledgement found.References
1. Paolilo, R.B., Deiva, K., Neuteboom, R., Rostasy, K. & Lim, M. Acute Disseminated Encephalomyelitis: Current Perspectives. Children (Basel) 7(2020).
2. Beatty, C., et al. Long-Term Neurocognitive, Psychosocial, and Magnetic Resonance Imaging Outcomes in Pediatric-Onset Acute Disseminated Encephalomyelitis. Pediatric neurology 57, 64-73 (2016).
3. Millward, J.M., et al. Transient enlargement of brain ventricles during relapsing-remitting multiple sclerosis and experimental autoimmune encephalomyelitis. JCI Insight 5(2020).
4. Evans, A.C. & Brain Development Cooperative, G. The NIH MRI study of normal brain development. NeuroImage 30, 184-202 (2006).
5. Richardson, H., Lisandrelli, G., Riobueno-Naylor, A. & Saxe, R. Development of the social brain from age three to twelve years. Nat Commun 9, 1027 (2018).
6. Billot, B., Colin, M., Arnold, S.E., Das, S. & Iglesias, J.E. Robust Segmentation of Brain MRI in the Wild with Hierarchical CNNs and no Retraining. ( arXiv:2203.01969, 2022).
7. Billot, B., et al. SynthSeg: Domain Randomisation for Segmentation of Brain Scans of any Contrast and Resolution. 19 ( arXiv:2107.09559 2021).
Figures