3522
Anomalous Neurovascular Coupling in cerebral small vessel disease patients related to cognitive impairment1Renji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Synopsis
Keywords: Dementia, Aging
NVC is thought to reflect the interrelationship between nutrient demand and supply, whereby neuronal activity influences local changes in blood flow. Injuries to the NVU could be the crucial point to CSVD, but the mechanisms remain obscure. This is the first study investigating CSVD from the perspective of the NVC at the whole brain, modular and regional levels.Introduction
Cerebral small vessel disease (CSVD) has an enormous impact on public health worldwide. Understanding the transition between non- cognitive impairment (CI) and CI state is vital for the management of CSVD patients. There is dynamic two-way communication between neurons and adjacent blood vessels, termed neurovascular coupling (NVC). The neurovascular unit, composed of neurons, glia, and vascular cells, is responsible for the NVC, which regulates local capillary blood flow to match oxygen and nutrient supply with current neural activity level and metabolic demands. There is evidence of NVC dysfunction in CSVD and it may precede normal clinical and imaging manifestations1. The aim of this study is to explore the underlying brain alterations of selective multiscale networks in CSVD patients related to cognitive impairment based on the method of NVC.Methods and materials
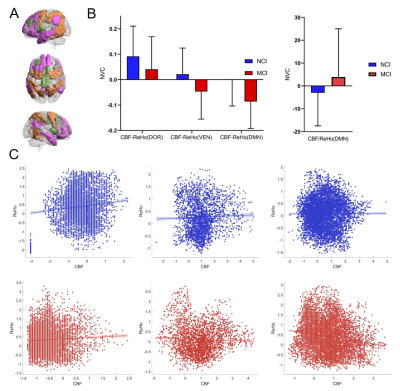
One hundred and twenty-four CSVD patients were enrolled, including 70 patients with mild cognitive impairment (MCI) and 54 patients with no cognitive impairment (NCI). Resting-state functional MRI and arterial spin labeling were explored to estimate the coupling of spontaneous neuronal activity and cerebral blood perfusion based on the amplitude of regional homogeneity (ReHo)-cerebral blood flow (CBF) correlation coefficients. The alterations of whole-brain gray matter, 9 subnetwork modules, and local NVC were evaluated by CBF-ReHo. Correlations between the NVC and neuropsychological assessments were explored in CSVD. Finally, we used these abnormal CBF-ReHo features in combination with machine learning to classify MCI and NCI.Results
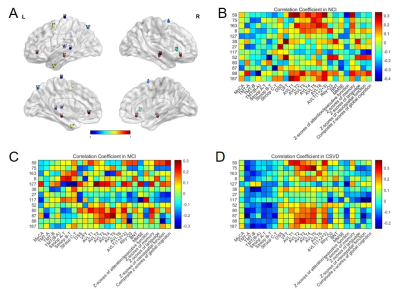
The NVC of the dorsal attention network (DOR), ventral attention network (VEN) and default mode network (DMN) in the MCI were significantly lower than those in the NCI. We also found a significantly abnormal CBF-ReHo predominantly located in cognitive-related brain regions, including subregions of the superior frontal gyrus, superior temporal gyrus, middle temporal gyrus, superior parietal gyrus, and cingulate gyrus. Moreover, the CBF-ReHo of the DOR, VEN, and DMN in the NCI group exhibited correlations with the executive function. The abnormal CBF-ReHo features achieved effective classification performance for MCI and NCI.Discussion and Conclusion
Decreased coupling in the DOR, VEN and DMN was found in MCI patients, which suggest changes in the above three modules may be the key to the transformation of cognitive function. Impaired VEN, DOR and DMN has been reported in patients with vascular MCI in prior work2,3. Our results also found that better executive function was associated with higher coupling in DMN and attention networks in NCI. The disproportionate NVC analysis at the regional level further specified the compromised coordination of NVU during the CSVD progression. An intriguingly decreased CBF-ReHo coefficient in subregions of middle temporal gyrus (MTG) and anterior cingulate cortex (ACC) of DMN, was discovered by using the index of regional neuronal activity. Moreover, MTG exhibit correlation with cognition function in CSVD and NCI. These are also consistent with a previous study showing that MTG allows the integration of automatic retrieval in the DMN with executively-demanding goal-oriented cognition4. By employing XGboost, we confirmed the superiority of multiscale NVC over single level NVC in the differential ability between CSVD patients with MCI and NCI.In conclusion, specific modular and regional NVC dysfunction of CSVD are linked to the onset and development of cognitive impairment. With the integrated BOLD and ASL approaches, the features of CBF-ReHo achieved efficient classification performance for differentiation between MCI patients and NCI. Eventually, characterizing NVC in CSVD at risk may aid in the development of targeted pharmacologic and neurotherapeutic treatment.
Acknowledgements
The authors sincerely thank all patients for their participation in this study.References
1. Monteiro A, Castro P, Pereira G, et al. Neurovascular Coupling Is Impaired in Hypertensive and Diabetic Subjects Without Symptomatic Cerebrovascular Disease[J]. Frontiers in aging neuroscience, 2021, 13.
2. Barrett A M, Boukrina O, Saleh S. Ventral attention and motor network connectivity is relevant to functional impairment in spatial neglect after right brain stroke[J]. Brain and cognition, 2019, 129: 16-24.
3. Yi L, Wang J, Jia L, et al. Structural and functional changes in subcortical vascular mild cognitive impairment: a combined voxel-based morphometry and resting-state fMRI study[J]. 2012.
4. Davey J, Thompson H E, Hallam G, et al. Exploring the role of the posterior middle temporal gyrus in semantic cognition: Integration of anterior temporal lobe with executive processes[J]. Neuroimage, 2016, 137: 165-177.
Figures