3464
Use of Dixon technique in breast contrast-enhanced T1WI for post-mastectomy patients at 3T1Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China, 2MR Collaborations, Siemens Healthineers Ltd., Chengdu, China, 3Philips Healthcare, Beijing, China
Synopsis
Keywords: Breast, Breast, MRI; Dixon; fat suppression; 3T
For patients with breast lesion resection, conventional contrast enhanced T1WI images with SPAIR provides poor fat suppression in the post-mastectomy breasts side due to the uneven skin surface, inhomogeneous tissues environment, and the frequency-selective feature of SPAIR scheme. Our study aimed to investigate the performance of fat suppression with the Dixon method in single side post-mastectomy patients. Subjective and objective evaluation suggested the Dixon method is superior to conventional SPAIR fat suppression in depicting the bilateral breast. Dixon method provided better image uniformity and higher fat suppression efficiency, and showed significant advantages in delineating the anatomical structures, with better axillary and lesion visibilities, especially in the completely removed breast side.Introduction/Purpose:
Contrast-enhanced T1WI (CE-T1WI) is widely used in breast MRI with high sensitivity in breast lesion detection, and high-quality fat suppression is essential for delineating of the enhanced lesions [1-2]. Conventionally, frequency-selective fat suppression with spectral attenuated inversion recovery (SPAIR) is routinely applied in clinical practice, but it suffers from inhomogeneous fat suppression, especially in the post-mastectomy breast side. This is related to uneven skin surface with contracted scars, field inhomogeneity in the broad contact area between the skin surface and surrounding air, SPAIR relies on frequency-selective excitation with lipid protons. Thus, poor fat suppression with SPAIR in post-mastectomy breast side makes it difficult for radiologists to give a definitive evaluation. Dixon method could achieve better fat suppression by reconstruction of in- and out-phase images which are less sensitive to B0 inhomogeneities [3]. Therefore, current study aims to investigate image quality and diagnostic performance of breast CE-T1WI with Dixon in post-mastectomy patients compared with SPAIR method.Materials and methods
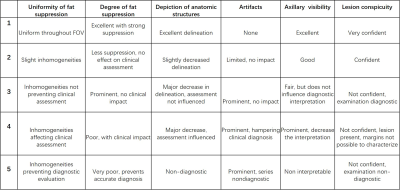
A total of 47 patients underwent mastectomy and post-operate breast CE-MRI were enrolled in this study. Both CE-T1WI with SPAIR and Dixon were scanned using a 3T MR scanner (Magnetom Skyra, Siemens Healthcare, Germany) with an 18-channel breast coil. Acquisition time of the two CE-T1WI with different fat-suppression methods were adjusted to be as similar as possible with the following parameters: SPAIR method: TR/TE=4.04/1.52ms, matrix size= 403x448, voxel size=0.8x0.8x0.8mm, TA=2min13s. Dixon method: TR/TE=5.52/2.46, 3.69ms, matrix size= 374x416, voxel size=0.87x0.87x0.90mm, TA=2min16s.Subjective evaluation was done by two independent experienced radiologists using a 5-point scale in consensus [4], with regards to fat-suppression efficiency and image uniformity, the visibility of anatomical structures and axillary nodes, lesion conspicuity, and severity of artifacts in bilateral breast sides (Table 1). For objective evaluation, CNR between enhanced lesions, ectopectoralis, and fat were calculated. The edge sharpness of the skin surface was measured in ImageJ software, which was defined as the mean slope of the signal intensity changes from post-operate skin surface to the subcutaneous fat. The bigger the value represents a greater edge sharpness. The uniformity in post-operative breast side was measured using 3D Slicer software and the Slicer-Radiomics extension (uniformity defined by IBSI as intensity histogram uniformity). The related ROIs were drawn to cover the left /right top quarter post-operative breast region and axillary region after the Dixon and SPAIR images were resampled to the same resolution and co-registered. The smaller the uniformity value represents the better fat suppression with good tissue/fat contrast. The uniformity values of the Dixon and SPAIR images were recorded for further comparison. Paired t-test and Wilcoxon rank sum test were used for statistical analyses.
Results:
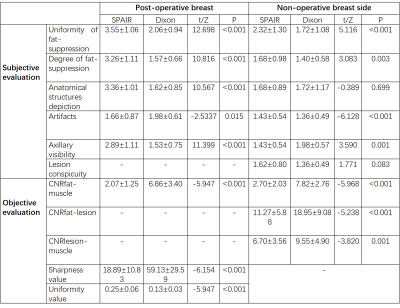
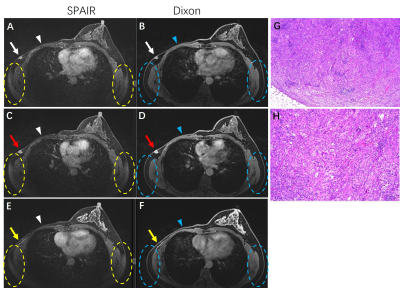
Subjective evaluationAs shown in Table 2, the Dixon method provided superior fat than the SPAIR method with significantly better subjective scores in regards to signal uniformity and degree of fat suppression (p<0.05) in a wide FOV range, including both in the post-operative & non-operative breasts and bilateral axillary areas (Fig 1-3). As for the anatomical structures’ definition, Dixon performed significantly better than SPAIR in the post-operative breast side with p<0.001, while there was no statistical difference for the non-operative breast side with p=0.699.
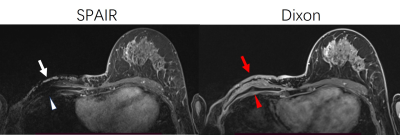
Although artifacts caused by cardiac impulse in SPAIR (1.66±0.87) were significantly less prominent than in Dixon (1.98±0.61) in the post-operative breast side, and in Dixon (1.36±0.49) was significantly better than in SPAIR (1.43±0.54) in the non-operative breast side with p <0.05, the scores were ranged from score 1 to 3, which did not deteriorate diagnostic confidence. As for axillary visibility, Dixon outperformed SPAIR in evaluation for both post- and non-operative breast sides with p<0.001 (Table 2).
For assessing the lesion conspicuity, Dixon performed similarly with SPAIR in the non-operative breast side with p=0.083 (Table 2), As for the post-operative breast side, there were 6 patients with abnormalities or enhancing lesions, statistical analysis was not performed due to the small sample size, the subjective scores for SPAIR and Dixon were listed as follows: 1,2,4,2,2,2 and 1,1,1,1,1,1, respectively. The incompletely and partially unsuppressed signals in the post-operative regions severely hindered the accurate depiction of anatomical structures and lesions (Fig 1-2), thus indicating the superior performance of the Dixon method.
Objective evaluation
As shown in Table 2, CNRs between fat, ectopectoralis, and lesions were significantly higher in images obtained by Dixon than by SPAIR (p<0.001), indicating better image contrast for evaluation. The edge sharpness between the skin surface and subcutaneous fat were significantly higher in Dixon than in SPAIR method (p<0.001). The signal uniformity of the post-operative breast side was seen with better fat suppression in Dixon than in SPAIR with p<0.001.
Additional findings
In 7 patients, the separation of water-only and fat-only images was incorrectly reconstructed, so nipples at one side or both two sides demonstrated fat-only signal in water-only images, and water-only signal in fat-only images, which would not interfere with the image interpretations of Dixon images.
Conclusions:
Dixon is superior to SPAIR with better image homogeneity of for fat suppression, and higher CNR for lesion depiction and image quality than SPAIR in bilateral breasts and axillary areas, especially in the postoperative breast through qualitative and quantitative assessment. Dixon is more advised to replace SPAIR in breast CE-T1WI for post-mastectomy patients.Acknowledgements
No acknowledgement found.References
1.Kuhl C. The current status of breast MR imaging. Part I. Choice of technique, image interpretation, diagnostic accuracy, and transfer to clinical practice. Radiology. 2007;244:356–78.
2.Niitsu M, Tohno E, Itai Y. Fat suppression strategies in enhanced MR imaging of the breast: comparison of SPIR and water excitation sequences. J Magn Reson Imaging. 2003;18:310–4
3.Glover GH (1991) Multipoint Dixon technique for water and fat proton and susceptibility imaging. J Magn Reson Imaging 1:521–530
4. Kalovidouri, A., Firmenich, N., Delattre, B.M.A. et al. Fat suppression techniques for breast MRI: Dixon versus spectral fat saturation for 3D T1-weighted at 3 T. Radiol med. 2017;122, 731–742.
Figures