3380
Influence of Financial and Socioeconomic Factors on MR Imaging Follow-up Time in Patients with Multiple Sclerosis1Department of Biomedical Engineering, Georgia Institute of Technology and Emory University, Atlanta, GA, United States, 2Department of Radiological Sciences, University of California, Irvine, Irvine, CA, United States, 3Department of Radiology and Imaging Sciences, Emory University School of Medicine, Atlanta, GA, United States, 4Department of Neurology, Emory University School of Medicine, Atlanta, GA, United States
Synopsis
Keywords: Multiple Sclerosis, Health Care Economics, Financial Toxicity, Imaging Follow-up Time
Multiple sclerosis (MS) is a chronic condition relying heavily on repeated MR imaging, and patients are particularly vulnerable to “financial toxicity”, a component of healthcare economics defined as the effects of healthcare costs on patient well-being. Our goal was to explore the effects of financial and socioeconomic factors on MRI follow-up time in patients with MS. Financial liability, or patient cost after primary insurance coverage, was associated with longer MRI follow-up time, suggesting financial toxicity may contribute to imaging frequency in MS patients. Further investigation over a longer time period is warranted.Introduction
Multiple sclerosis (MS) is an autoimmune disease affecting the central nervous system and characterized by chronic inflammation and demyelination of the nervous system1. Both diagnosis and prognosis of MS rely heavily on MRI, with current diagnostic guidelines requiring confirmation of hyperintense lesions on T2-weighted/FLAIR brain images. Furthermore, clinical guidelines recommend repeated brain MRI as frequently as every 6-12 months. Post-diagnosis, imaging is recommended prior to starting new disease-modifying treatment and every 1-2 years, depending on treatment type2. The high cost of disease-modifying therapies and medical imaging particularly in the United States healthcare system, combined with the chronic and lifelong nature of MS, results in high risk for “financial toxicity”, or the effects of the financial burden of disease-associated costs on patient well-being. Financial toxicity has been shown to be associated with non-adherence to care plans including imaging3,4, and missed or delayed imaging can compromise patient outcomes. The goal of this study was to determine effects of financial and socioeconomic factors, including financial liability, area deprivation index (ADI), and insurance status, on MRI follow-up time.Methods
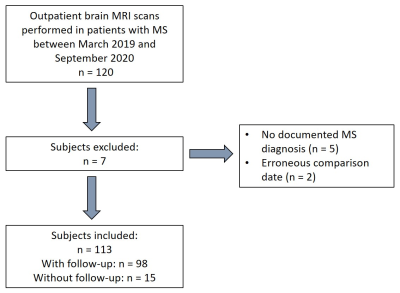
This retrospective study was approved by the local Institutional Review Board. All brain MRI scans performed within our hospital system during an 18-month period between March 2019 – September 2020 were reviewed. Inclusion criteria were outpatient scans performed for clinical indication of MS in patients ≥18 years old. Follow-up time between scans, or absence of follow-up, was determined from radiology reports. Exclusion factors included erroneous scan comparison dates and no documented MS diagnosis in electronic medical records (Figure 1). For included subjects, financial data including financial liability (remaining costs, in dollars, after primary insurance coverage), insurance type (public, private, or unknown), and presence of unpaid medical debt were obtained from the hospital billing department. Demographics were acquired from medical records including gender, race, home address, and 5-digit zip code. Addresses and 5-digit zip codes were used to determine 9-digit zip codes using the United States Postal Service database and matched with national ADI scores, a metric of socioeconomic status, using the Wisconsin Neighborhood Atlas5. Clinical data was obtained from medical records including John Cunningham (JC) virus status and use of natalizumab as part of treatment.Statistical analyses were performed in SPSS 28.0. Normality was evaluated using Kolmogorov-Smirnov tests. National ADI scores (1-100) were stratified into quintiles based on equal group sizes, with higher scores indicating more disadvantage. Group-wise comparisons of follow-up time as a function of the presence of unpaid medical debt and insurance type were performed using Mann-Whitney U tests, and as a function of ADI quintiles using a Kruskal-Wallis test. Linear regression analyses were used to identify associations between length of follow-up time (days) and financial and socioeconomic factors, with gender, race, JC virus status, and natalizumab as categorical covariates. Financial liability was stratified as zero or non-zero and also used as a covariate. The log10 of follow-up time (days) and log10 financial metrics were used in regression analysis to address non-normality of data. Significance was determined by p ≤ .05 for all analyses.
Results
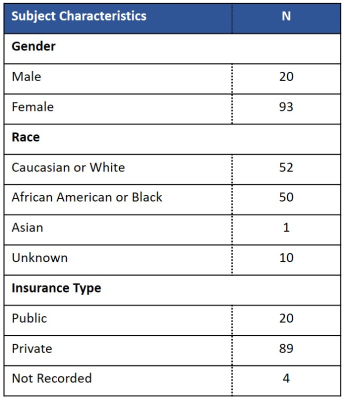
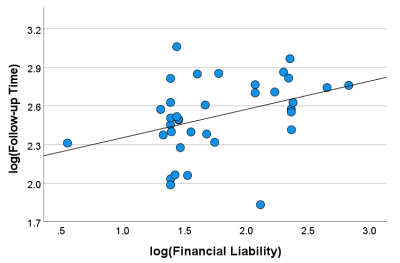
A total of 113 subjects were included (mean ± standard deviation age 43.5 ± 13.1 years; 93 female and 20 male, Figure 2). Of the 113 subjects, 98 had follow-up scans with a median ± interquartile range follow-up time of 335 ± 294 days. Group-wise comparisons revealed no significant differences in follow-up time as a function of insurance type or presence/absence of unpaid medical debt. The mean national ADI scores for our cohort were 48 ± 25, and no significant differences in follow-up time were observed between ADI quintiles. For financial metrics, a significant difference in follow-up time was observed for subjects with no financial liability and those with non-zero financial liability (p= 0.010). Post-hoc regression analysis for patients with non-zero financial liability revealed a significant relationship between follow-up time and amount of financial liability for the earlier scan (R = 0.375, p = .025, Figure 3). The remaining covariates (gender, race, JC virus status, or use of natalizumab) were not significant in regression analysis.Discussion
The effects of socioeconomic status on clinical decision making are well documented6. In MS, lower socioeconomic status has been associated with increased difficulty in accessing disease-modifying treatments7. Our results suggest financial liability is associated with longer MRI follow-up times in MS. Interestingly, we did not observe differences in follow-up for patients with difference types of insurance or higher ADI scores; however, we note the time period for our study (March 2019 – September 2020) may have been affected by reductions in elective procedures due to COVID-19. The size of our cohort was relatively small due to the time period of the study, and replication in a larger cohort over a longer time period is warranted.Conclusion
Increased financial liability resulting from MRI services is associated with longer MRI follow-up time in MS. Future work will explore additional factors in a larger cohort including proximity to care facilities, familial support, and financial security.Acknowledgements
We would like to acknowledge Abinand Rejimon for assistance with obtaining clinical data. R.A. received support from the Georgia Tech President’s Undergraduate Research Award to conduct this research.
References
1. Tafti, D., Ehsan, M., & Xixis, K. L. (2022). Multiple Sclerosis. In StatPearls. Accessible at https://pubmed.ncbi.nlm.nih.gov/29763024/
2. Kaunzner, U. W. & Gauthier, S. A. (2017). MRI in the assessment and monitoring of multiple sclerosis: an update on best practice. Ther Adv Neurol Disord, 10(6), 247-261.
3. Desai, A. & Gyawali, B. (2020). Financial toxicity of cancer treatment: Moving the discussion from acknowledgement of the problem to identifying solutions. EClinicalMedicine, 20, 100269.
4. Sadigh, G. Lava, N., Switchenko, J., Duszak, R. Jr, Krupinski, E. A., Meltzer, C., Hughes, D., & Carlos, R. C. (2021). Patient-reported financial toxicity in multiple sclerosis: Predictors and association with care non-adherence. Mult Scler, 27(3), 453-464.
5. Kind, A. J. H. & Buckingham, W. R. (2018). Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N Engl J Med, 378(26), 2456-2458.
6. Bernheim, S. M., Ross J. S., Krumholz H. M., & Bradley E. H. (2008). Influence of patients' socioeconomic status on clinical management decisions: a qualitative study. Ann Fam Med, 6(1), 53-9.
7. Calocer, F., Dejardin, O., Droulon, K., Launoy, G., & Defer, G. (2018). Socio-economic status influences access to second-line disease modifying treatment in Relapsing Remitting Multiple Sclerosis patients. PLoS One, 13(2), e0191646.
Figures