3368
A multicentric validation of cerebral morphologic changes in menopausal women: DARTEL-based voxel-based morphometry (VBM) study
Tae-Hoon Kim1, Youe Ree Kim2, Chang-Won Jeong1, ByoungRyun Kim3, Chungsub Lee1, SiHyeong Noh1, DongWook Lim1, and Young Hwan Lee2
1Medical Convergence Research Center, Wonkwang University, Iksan, Korea, Republic of, 2Radiology, Wonkwang University School of Medicine and Hospital, Iksan, Korea, Republic of, 3Obstetrics and Gynecology, Wonkwang University School of Medicine and Hospital, Iksan, Korea, Republic of
1Medical Convergence Research Center, Wonkwang University, Iksan, Korea, Republic of, 2Radiology, Wonkwang University School of Medicine and Hospital, Iksan, Korea, Republic of, 3Obstetrics and Gynecology, Wonkwang University School of Medicine and Hospital, Iksan, Korea, Republic of
Synopsis
Keywords: Gray Matter, Aging, menopause
Among recent voxel based-morphometry (VBM) technique, DARTEL (Diffeomorphic Anatomical Registration Through Exponentiated Lie Algebra)-based VBM method can provide powerful information to understanding morphologic variations in whole brain areas. In women, several VBM studies reported unveiling the brain morphologic reductions (putamen, pallidum, hippocampus, postcentral gyrus, frontal/paritetal/temporal gyrus, and so on) after menopause. These studies provided menopause-related brain centers in postmenopausal women; however these morphologic findings might be included potentially case-sensitive results as a consequence of the enrolled population. This study was performed a multicentric study to evaluate cerebral morphological changes in menopausal women by using a DARTEL-based VBM method.Introduction
Among recent voxel based-morphometry (VBM) technique, DARTEL (Diffeomorphic Anatomical Registration Through Exponentiated Lie Algebra)-based VBM method can provide statistically powerful information to understanding morphologic variations in whole brain areas. During menopause transition, VBM method allowed unveiling the brain morphologic changes after menopause by the recession of the supply of follicles [1-3]. Several VBM studies reported the morphologic reductions (putamen, pallidum, hippocampus, postcentral gyrus, frontal/paritetal/temporal gyrus) after menopause [2-4]. These studies elucidated specific brain centers on menopause-related morphological changes; however these morphologic findings might be included potentially case-sensitive results as a consequence of the enrolled population in each institution. Therefore, this study was performed a multicentric study to evaluate cerebral morphological changes in menopausal women by using a DARTEL-based VBM method.Subjects and Methods
A total of seventy-two subjects were enrolled at Wonkwang University Hospital (WKUH) (n=24, premenopause 14; menopause 10) and Chonnam National University Hospital (CNUH) (n=48, premenopause 24; menopause 24). Menopause was defined as continuous amenorrhea for more than 12 months and FSH level more than 30 mIU/mL. Both groups have no history of hormone therapy and neurological illness. All participants underwent blood testing for comparing the sex hormone levels. The measured sex hormones included anti-mullerian hormone, total estrogen, estradiol, testosterone, progesterone, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and sexual hormone-binding globulin (SHBG).MR imaging examinations were obtained using 3T MRI scanners at WKUH (Achieva; Philips) and CNUH (Magnetom Trio; Siemens). The imaging parameters were as follows: TR/TE = 8.1/4.6 ms, FOV = 256 × 256 × 180 mm2, flip angle = 8°, slices = 180, voxel size = 1×1×1 mm3, acquisition time = 4 minutes 32 seconds. Brain images were acquired using the 3-dimensional T1-weighted acquisition (MP-RAGE). MRI data were processed by using SPM12 with DARTEL algorithm: segmentation, normalization, modulation and smoothing 6 mm FWHM Gaussian kernel. The variation of brain volume between premenopausal and menopausal women was analyzed by two sample t-test. Significant brain areas were quantified using customized expert system for quantification of brain activation (QUBA) software as shown in Fig. 1.
Results
Table 1 compares the mean sex hormonal levels in premenopausal and menopausal women. The levels of the anti-mullerian hormone, total estrogen, estradiol, testosterone, progesterone, FSH, and LH were significantly different between two groups (p<0.01). Especially, the total estrogen and estradiol in menopausal women showed lower levels than that in premenopausal women, whereas the levels of FSH and LH are higher in menopausal women. These hormonal levels in menopausal women showed similar changing patterns at both centers.Figure 2 shows the significantly reduced GM volumes in menopausal women at two medical centers and their localized areas are summarized in Table 2 and Fig. 3. However, there was no increased GM volume in the menopausal women.
Conclusion
This study finds out the reproducible localized brain volume changes following menopause at two medical centers. These anatomical areas would be useful for an understanding of an interaction by the brain volume changes and the levels of sex hormones following menopause.Acknowledgements
This study was supported by the grants of the NRF (2020R1I1A1A01073871) and KHIDI, funded by the Ministry of Health &Welfare (HI18C1216).References
1. Lu W, et al., J Neuroendocrinol. 2018; 30(12): e12655.
2. Lord C, et al., Menopause. 2010; 17(4): 846-51.
3. Zhang T, et al., PLoS One. 2016; 11(3): e0150834.
4. Boyle CP, et al., Human Brain Mapping. 2021; 42: 24-35.
Figures
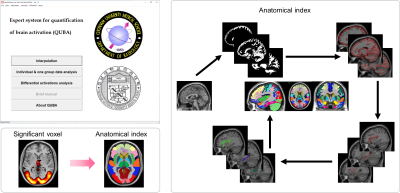
Figure 1. Expert system for quantification of brain activation (QUBA) software and flowchart of quantification procedures.
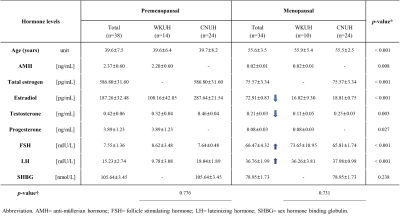
Table 1. Serum
sex hormone levels in premenopausal and menopausal women at two medical centers
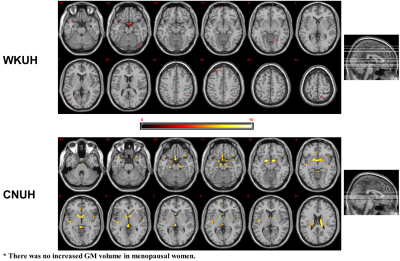
Figure 2. Axial multi-slice images of localized brain
volume reductions in menopausal women, which analyzed with two sample t-test (p<0.001; cluster size 10): Wonkwang University Hospital (WKUH)
and Chonnam National University Hospital (CNUH).
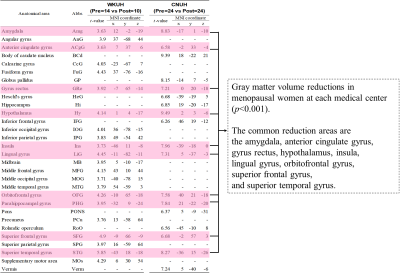
Table 2. GM volume reduction areas in menopausal women at two different centers (p<0.001)
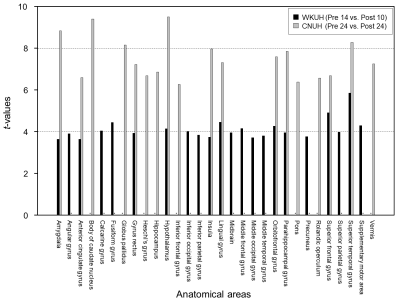
Figure 3. Gray matter volume changes in menopausal women at each medical center (p<0.001). The common reduction areas
are as follows: the amygdala, anterior cingulate gyrus, gyrus rectus,
hypothalamus, insula, lingual gyrus, orbitofrontal gyrus, superior frontal
gyrus, and superior temporal gyrus.
DOI: https://doi.org/10.58530/2023/3368