3334
Functional Connectivity between Right Rolandic Operculum and Default Mode Network Is Associated with Chronic Low Back Pain-Related Disability1Institute of Medical Device and Imaging, National Taiwan University, Taipei, Taiwan, 2Department of Physical Therapy, National Taiwan University, Taipei, Taiwan, 3Department of Surgery, National Taiwan University, Taipei, Taiwan
Synopsis
Keywords: Brain Connectivity, fMRI (resting state)
This study aimed to explore the relationship between emotion and pain-related disability in patients with chronic low back pain (CLBP) by using resting-state functional connectivity (FC). Our results showed that as compared with the control group (n = 26), the patient group (n = 26) had decreased FC with the default mode network in multiple brain regions. Specifically, the right Rolandic operculum was identified, where FC was inversely correlated with the Oswestry disability index (r = -0.616, p < 0.001), suggesting the interplay between emotion processing and pain perception.Purpose
Chronic low back pain (CLBP) is a common health condition in adults and a leading cause of disability1, 2. In patients with CLBP, changes in emotion and cognition have been reported3, and altered functional connectivity (FC) was found in brain regions responsible for cognition4. However, the relationship between emotion and pain-related disability was less explored. Based on the knowledge that emotion and cognition can modulate pain perception5, we hypothesize that the FC in brain regions associated with emotion is different between healthy controls and patients with CLBP.Materials and Method
Twenty-six CLBP patients and 26 healthy volunteers were recruited. MR images were acquired on a 3-Tesla whole-body scanner (Prisma, Siemens). Imaging protocol included 3D T1-MPRAGE (voxel size = 0.9x0.9x0.9 mm3) and resting-state blood oxygenation level dependent (BOLD) imaging (TR/TE = 2000/24 ms, voxel size = 3.0x3.0x3.5 mm3, 210 measurements).By using the Statistical Parametric Mapping software (www.fil.ion.ucl.ac.uk/spm/software/spm12/), BOLD images were corrected for slice timing and head motion, and normalized to the Montreal Neurological Institute space after coregistration with anatomical images. The normalized images were smoothed with an isotropic Gaussian kernel of 6-mm full width at half maximum. For each voxel, nuisance noise, estimated from motion parameters, white matter signal, and ventricular signal, was removed from the signal time curve using the anatomical component correction (aCompCor)6 algorithm, the residual signal of which was then band-pass filtered to retain the frequency range of 0.008 to 0.08 Hz. The posterior cingulate cortex, the hub of the default mode network (DMN), was chosen to be the seed by using the automatic anatomical labeling atlas7. The average signal time curve within the seed was correlated with the signal time curve of every voxel. The Fisher’s z-transformed Pearson’s correlation coefficient was used as the measure of FC with DMN. The FC difference between groups was voxel-wise examined using the two sample t-test and the following criteria: p < 0.001 and a cluster size > 25 mm3. Linear regression was used to examine the correlation between FC and symptom severity assessed by the Oswestry disability index (ODI), visual analogue scale (VAS), time-up-and-go test (TUG test) and sit-to-stand test.
Results and Discussion
Table 1 summarizes the four clusters identified by two-sample t-test where FC with DMN is different between groups (Table 1). Figure 1 shows the FC values in each of the clusters. Among the clusters, linear correlation analysis shows a significant negative correlation between ODI and the FC in the right Rolandic operculum (Table 2 and Figure 2), a region previously shown to involve in emotion processing8.It is worth noting that ODI is a multidimensional scale for measuring the disability of low back pain9, 10. The observed alteration in emotion processing may interfere with pain-related disability through one or both of the following mechanisms: (1) the indirect mechanism where less emotional suppression increases pain perception; (2) the direct mechanism where negative emotion causes negative self-rating on disability questionnaire.
Conclusions
This study reported altered FC in multiple brain regions in patients with CLBP. Decreased FC in the right Rolandic operculum, a region associated with emotion processing, was found to correlate with increased pain-related disability as evaluated by ODI. Further study with a larger population and more comprehensive neurological scales is warranted to enhance the neuropathological interpretability.Acknowledgements
This study was supported by Ministry of Science and Technology, Taiwan (107-2221-E-002-069-MY3; PI: Wang SF), and National Health Research Institute, Taiwan (EX101-10142E1; PI: Wang SF).
References
1. Hartvigsen, J., et al., What low back pain is and why we need to pay attention. Lancet, 2018. 391(10137): p. 2356-2367.2. Maher, C., M. Underwood, and R. Buchbinder, Non-specific low back pain. Lancet, 2017. 389(10070): p. 736-747.
3. Ng, S.K., et al., The Relationship Between Structural and Functional Brain Changes and Altered Emotion and Cognition in Chronic Low Back Pain Brain Changes: A Systematic Review of MRI and fMRI Studies. Clin J Pain, 2018. 34(3): p. 237-261.
4. Čeko, M., et al., Partial recovery of abnormal insula and dorsolateral prefrontal connectivity to cognitive networks in chronic low back pain after treatment. Human brain mapping, 2015. 36(6): p. 2075-2092.
5. Price, D.D., G.N. Verne, and J.M. Schwartz, Plasticity in brain processing and modulation of pain. Prog Brain Res, 2006. 157: p. 333-352.
6. Behzadi, Y., et al., A component based noise correction method (CompCor) for BOLD and perfusion based fMRI. Neuroimage, 2007. 37(1): p. 90-101.
7. Tzourio-Mazoyer, N., et al., Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage, 2002. 15(1): p. 273-89.
8. Sutoko, S., et al., Lesions in the right Rolandic operculum are associated with self-rating affective and apathetic depressive symptoms for post-stroke patients. Sci Rep, 2020. 10(1): p. 20264.
9. Lee, C.P., et al., Psychometric evaluation of the Oswestry Disability Index in patients with chronic low back pain: factor and Mokken analyses. Health Qual Life Outcomes, 2017. 15(1): p. 192.
10. Vianin, M., Psychometric properties and clinical usefulness of the Oswestry Disability Index. J Chiropr Med, 2008. 7(4): p. 161-3.
Figures

Table 1. The brain regions where functional connectivity with the default mode network is statistically different between control and patient groups.
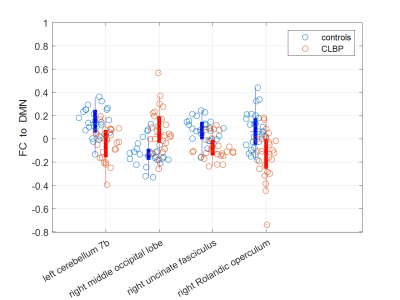
Figure 1. The values of functional connectivity (FC) with the default mode network (DMN) within the brain regions where statistical difference is found between controls and patients with chronic low back pain (CLBP).
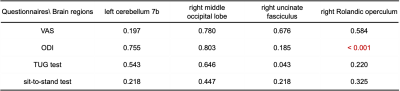
Table 2. The p-values of linear correlation analysis between functional connectivity and scales of low back pain-related symptom severity. The statistically significant correlation is labeled in red. VAS = visible analogue scale, ODI = Oswestry disability index, TUG test = time-up-and-go test.
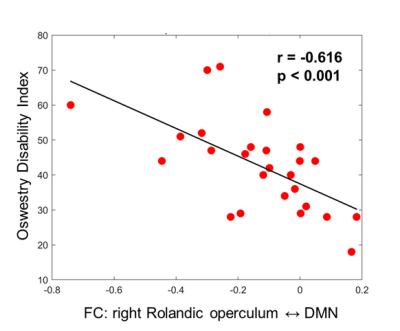
Figure 2. Scatter plot of Oswestry disability index with respect to functional connectivity (FC) between right Rolandic operculum and default mode network (DMN).