3303
Disruptions in regional homogeneity and functional connectivity relate to subacute ischemic stroke1Xi'an Daxing Hospital, Xi'an, China
Synopsis
Keywords: Stroke, fMRI (resting state)
The primary aim of the research was to compare the impact of subacute ischemic stroke on brain activity using resting state functional magnetic resonance imaging. In this study, we applied ReHo and FC to investigate the characteristics of brain functional activity in subacute ischemic stroke patients. Our results showed that the subacute ischemic stroke patients showed increased ReHo values in the left postcentral gyrus and significantly decreased FC between the Cerebellum-SUIT_7 and the right caudate, which is beneficial to understand the neurophysiological mechanisms of subacute ischemic stroke.Introduction
Ischemic stroke remains one of the major causes of disability and death throughout the world 1. With the continuous development of neuroimaging technology, neuroimaging diagnosis has entered a comprehensive diagnosis stage combining brain morphology and function. A previous study found focal cortical atrophy in areas of frontal and temporal cortices in subacute ischemic stroke patients 2. Resting state fMRI methods include functional segregation (regional homogeneity, ReHo) and functional integration (seed-based functional connectivity analyses, FC) for studying brain function. The purpose of present study was to investigate alterations of brain functional activity in subacute ischemic stroke patients utilizing ReHo and FC.Methods
Twenty-five ischemic stroke patients (male 18, mean age 57.12±11.24) and 28 healthy controls (male 18, mean age 57.61±7.13) were recruited for this cross-section fMRI study. MRI data were acquired on a 3.0 T MRI scanner using a 64-channel head and neck coil. Resting state fMRI data were obtained using gradient echo-echo planar imaging pulse sequence with TR=720 ms, TE=33.1 ms, flip angle=52 °, matrix=104 × 90, FOV=208 mm×180 mm, slice thickness=2 mm, 72 slices. The fMRI images were preprocessed using Matlab R2019a, BPABI_V6.1 and SPM12 software. The fMRI data were corrected by time and head motion, resampled into voxels of 3 × 3 × 3 mm3 and normalized to Montreal Neurological Institute (MNI) template, then smoothed, linear drifted and band filtered (filtering frequency of 0.01 ~ 0.1 Hz), finally ReHo values were analyzed. Difference in ReHo values between groups were analyzed using two-sample t test. Pearson correlation analysis was used to explore the relationships between the ReHo values and clinical indices in ischemic stroke patients. To calculate seed-based functional connectivity between groups, we defined 44 regions of interest (ROIs) with 6 mm diameter spheres.Results
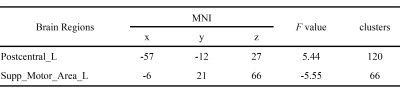
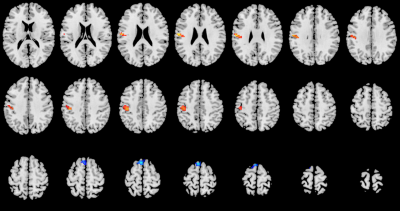
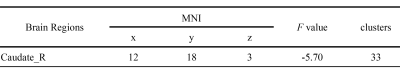
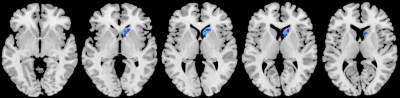
There were no significant differences between the two groups in their age (t=-0.19, P=0.85) and gender (χ2=0.36, P=0.55). In comparison with healthy controls, increased ReHo values appeared mainly in the left postcentral gyrus, and significantly decreased ReHo values in the left supplementary motor area in subacute ischemic stroke patients (single voxel P<0.001, GRF corrected). There were no significant associations between the ReHo values and clinical indices (P>0.05). Compared with healthy controls, subacute ischemic stroke patients showed significantly decreased (single voxel P<0.001, GRF corrected) FC between the ROI (Cerebellum-SUIT_7) and the right caudate (MNI coordinates: 12, 18, 3; peak t value: -5.70; cluster size: 33 ml).Discussion
The most common symptom related to ischemic stroke is sensorimotor dysfunction 3. The present study found that increased ReHo values appeared mainly in the left postcentral gyrus in subacute ischemic stroke patients. As an important component of the sensorimotor network, the postcentral gyrus is strongly associated with motor impairment after stroke 4, which may explain the sensorimotor dysfunction following ischemic stroke. Meanwhile, there was significantly decreased FC between the Cerebellum-SUIT_7 and the right caudate. The caudate is an associative structure, which has been involved in motor, behavior, and dysexecutive disorders due to its important connections with the frontal and parietal lobes 5, which provided valuable information for exploring the pathological mechanisms of subacute ischemic patients.Conclusion
Our results indicated that regional brain functional activity is impaired in subacute ischemic patients. These findings will provide further insight into the neurophysiological mechanisms of ischemic stroke.Acknowledgements
No acknowledgement found.References
1. Fukuta T, Oku N, Kogure K. Application and Utility of Liposomal Neuroprotective Agents and Biomimetic Nanoparticles for the Treatment of Ischemic Stroke. Pharmaceutics. 2022; 14(2): 361.
2. Yan S, Zhang G, Zhou Y, et al. Abnormalities of Cortical Morphology and Structural Covariance Network in Patients with Subacute Basal Ganglia Stroke. Acad Radiol. 2022; Suppl 3: S157-S165.
3. van der Vliet R, Selles RW, Andrinopoulou ER, et al. Predicting Upper Limb Motor Impairment Recovery after Stroke: A Mixture Model. Annals of Neurology. 2020; 87: 383-393.
4. Xu H, Qin W, Chen H, et al. Contribution of the resting-state functional connectivity of the contralesional primary sensorimotor cortex to motor recovery after subcortical stroke. PLoS One. 2014; 9(1): e84729.
5. Rosso C, Blanc R, Ly J, et al. Impact of infarct location on functional outcome following endovascular therapy for stroke. J Neurol Neurosurg Psychiatry. 2019; 90(3): 313-319.
Figures