3290
Amide Proton Transfer-Weighted MRI in Preoperative Assessment of Microvascular Invasion of Hepatocellular Carcinoma: A Preliminary Study1Clinical Medical School of Yangzhou University, Northern Jiangsu People’s Hospital, Yangzhou, China, Yangzhou City, China, 2GE Healthcare, MR Research China, Beijing, P.R. China, Beijing City, China
Synopsis
Keywords: Quantitative Imaging, CEST & MT, APTw
Conventional MRI methods are difficult to reveal histologic and molecular characteristic of HCC. In this study, we aimed to e explore the feasibility of amide proton transfer weighted (APTw) imaging for predicting microvascular invasion (MVI) of hepatocellular carcinoma. Significant difference in APTw values were observed for MVI positive and negative lesions. With these findings, APTw imaging can be considered a potential technique for noninvasive preoperational assessment of MVI in hepatocellular carcinoma.Introduction
Hepatocellular carcinoma (HCC) is the fastest rising cause of cancer-related death worldwide. Surgical resection and liver transplantation remain as the first-choice treatments for patients with early-stage HCC. MVI mainly appears as small thrombi of malignant cells in the portal and hepatic venous systems. And MVI had been demonstrated as a strong risk factor associated with recurrence and survival among HCC patients after resection[1]. However, currently, MVI can only be reliably determined by histopathologic evaluation of surgical specimens.Amide proton transfer weighted (APTw) imaging, as a branch of chemical exchange saturation transfer (CEST) imaging, focuses on proton exchange between amide protons of peptides and proteins and bulk water[2,3]. Two recent studies showed the potential of APTw imaging in predicting the histologic grades of HCC[4,5]. Moreover, some histological differentiation of HCC had strong relationship with MVI, in other words, MVI was more easily presented in patients with worse histological differentiation. With these applications, we hypothesized that APTw imaging may help to assess the MVI of HCC.
Materials and Methods
SubjectsThe study was approved by local ethical community and consent forms were obtained from all patients. 32 patients histologically confirmed HCC were enrolled in the study. MVI was pathologically confirmed from tumor resection including 13 cases with MVI (MVI+) and 15 without MVI (MVI−).
MRI experiments
All patients underwent liver MR scanning on a 3.0-tesla scanner (GE DISCOVERY MR750; Milwaukee, Wisconsin, USA) with a 32-channel phased-array torso coil. All patients underwent fasting 4-6 hours before examination. Liver tumor scan protocol was used including routine T2 weighted imaging, T1 weighted imaging, diffusion-weighted imaging. Before contrast injection, APTw imaging was performed with a respiratory triggered single slice Spin-echo echo-planar-imaging sequence. Images at 52 frequencies were acquired, including 49 frequencies ranging from -600 to 600 Hz with an increment of 25 Hz. The applied saturation B1 power was 2µt and the saturation duration was 2000ms. Other scan parameters were of TE=32.7ms, TR=5432ms, FOV=34cm × 26 cm, Matrix size=128 × 128, and slice thickness=8mm. Scan time was around 2 minutes 52 seconds.
Imaging analysis
Magnetization transfer ratio asymmetry (MTRasym) image at 3.5ppm was obtained for each patient. Two radiologists with 5 and 13 experiences were employed for data analysis. With the reference of axial T2WI images, three circular regions of interest (ROIs) with approximately 40-50mm2 were placed manually in the solid component of the tumor for each patient on unsaturated M0 images. Large cystic cavities, large areas of necrosis, calcification, hemorrhage, and large vessels were excluded from ROI selections. ROIs of tumors were copied on the MTRasym map. Then the average APTw in the three ROIs for each radiologist was obtained for subsequent analyses.
Statistical analysis
All statistical analyses were performed in SPSS 23.0. The inter-class correction coefficient (ICC) was used to evaluate the inter-observer agreement of measuring APTw value between two radiologists. ICC>0.75 was considered good reproducibility. The comparisons between APTw value for MVI- and MVI+ groups were analyzed using the independent t test. Receiver operating characteristic (ROC) curves were generated for each APTw parameter value to assess the areas under the curve (AUC).
Results
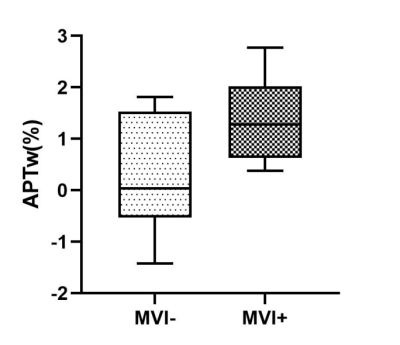
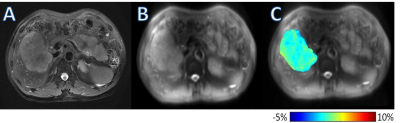
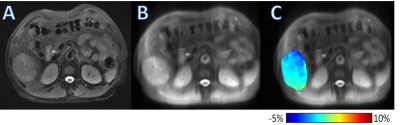
The ICC of two observers’ measurements was 0.912. The APTw value of MVI+ group was significantly higher than that of MVI− group [ (1.33±0.76) % vs (0.32±1.06) %; P=0.008] (Fig. 1). The cut-off APTw value for differentiating MVI+ and MVI− groups was 0.30% (sensitivity, 60%; specificity, 100%; AUC, 0.782, 95%CI: 0.609, 0.955). Representative cases are shown in Fig. 2 and Fig. 3.Discussion and conclusions
Our study showed that the APTw value of MVI+ group is significantly higher than MVI- group. Hepatocellular carcinoma with microvascular invasion tends to be more malignant and has more mobile proteins and may have a higher proliferation of hepatocellular carcinoma cells, greater cell density, which leads to the higher value of APTw.In conclusion, this study showed promising ability in differentiating MVI+ and MVI− HCC. Follow-up studies with larger patient cohort are needed to further validate its diagnostic performance.
Acknowledgements
We thank Weiqiang Dou from GE Healthcare for this valuable support on APT sequences.References
1 Du M, Chen L, Zhao J, et al. Microvascular invasion (MVI) is a poorer prognostic predictor for small hepatocellular carcinoma. BMC Cancer. 2014;14:38.
2 Zhou J, Payen JF, Wilson DA, Traystman RJ, van Zijl PC. Using the amide proton signals of intracellular proteins and peptides to detect pH effects in MRI. Nat Med. 2003;9(8):1085-1090.
3 Zhou J, Lal B, Wilson DA, Laterra J, van Zijl PC. Amide proton transfer (APT) contrast for imaging of brain tumors. Magn Reson Med. 2003;50(6):1120-1126.
4 Wu B, Jia F, Li X, Zhang M, Han D, Jia Z. Amide Proton Transfer Imaging vs Diffusion Kurtosis Imaging for Predicting Histological Grade of Hepatocellular Carcinoma. J Hepatocell Carcinoma. 2020;7:159-168. 5 Lin Y, Luo X, Yu L, et al. Amide proton transfer-weighted MRI for predicting histological grade of hepatocellular carcinoma: comparison with diffusion-weighted imaging. Quant Imaging Med Surg. 2019;9(10):1641-1651.
Figures