3267
An optimal multiple b-value scheme for applications in female cervical cancer1Department of Biomedical Engineering, Hubei University of Medicine, Hubei, China, 2GE Healthcare, Beijing, China, 3Department of Radiology,Taihe Hospital, Hubei University of Medicine, Hubei, China
Synopsis
Keywords: Uterus, Cancer
Incoherent motion in voxel (IVIM) imaging is widely utilized in grading tumor, cancer, treatment efficacy and prognosis. It is believed utility of at least 8 b-values image sets brings a more stable and accurate results. However, long acquisition time hamper clinical applications. High consistent diagnostic performance of manual ROI-based IVIM-derived measurements including ADC, D, D* and f on distinguishing patients with cervical cancer from healthy controls was found between 5b-value and 13b-value IVIM imaging protocol and no significant difference of all four values was found. We proposed a IVIM diffusion weighted imaging with a 5b-value protocol in cervical cancer.Introduction
Incoherent motion in voxel (IVIM) imaging is an extension of diffusion-weighted imaging (DW-MRI) [1] and has been applied to grade cervical tumors and predict the efficacy of radiotherapy and chemotherapy with higher accuracy, sensitivity and specificity than conventional DW-MRI. Slow diffusion coefficient (D), fast diffusion coefficient (D*) and perfusion fraction (f) is computed based on a bi-exponential equation Sb/S0=(1-f)×exp(-bD)+f×exp[-b×(D+D*)] , where Sb is the signal intensity at b-value is greater than 0 s/mm2, S0 is the signal intensity at b-value is 0 s/mm2. These quantitative values reflects pure water diffusion and microcirculation perfusion in tumor [2,3]. It is believed utility of more b-value images, at least 8 b-values, brings a more stable and accurate results [4, 5]. However, acquisition prolongs as the number of and the strength of used b-values, leading to difficulty in wide clinical applications. Few studies of cervical cancer using IVIM reported that various cutoff values were obtained from IVIM model using different b-values, leading to unstable diagnostic performance and treatment selection. Therefore, we aimed to explore a set of b-values for build an IVIM model with short scan time, consistent quantitative parameters, and equivalent diagnostic efficacy in cervical cancer.Materials and methods
We prospectively recruited 35 cervical cancer patients, 35 healthy volunteers in our hospital from May to November 2021. All patients were instructed to empty the bladder appropriately to reduce intestinal peristalsis artifacts and urine electrolyte artifacts and underwent routine MRI scan and an IVIM sequence (TR/TE =4000/71.6ms, FOV = 22 cm, thickness =4 mm, 13b= 0, 25, 50, 75, 100, 150, 200, 400, 600, 800, 1000, 1200 and 1500 s/mm2) on 1.5T MRI (Signa voyager, GE Healthcare) with 8-channel abdominal phased coil in a total of 11’12’’ scan time. All IVIM data were transferred to Advanced Workstation 4.6 (GE Healthcare) and analyzed with a bi-exponential model to obtained D, D* and f values for different number of b-value protocols (5, 7, 8, 9, 10, 13 b-value sets). Two experienced radiologists double-blind sketched the largest cross-section level of lesions using T2WI as reference with care avoiding the areas of blood vessels, tumor bleeding and necrosis. ROIs were copied to the same slice of different b-value computed ADC, D, D* values and f maps to obtained all measurements. All data were presented in mean±standard deviation (xˉ±s) and statistical analysis was performed using SPSS26.0 (IBM, Armonk, NY). Paired t-test or Wilcoxon sign test was used for comparison between different b-value maps according to normality and equality-of-variances respectively examined by Kolmogorov-Smirnov test and Levene's-Test. Receiver operating characteristic (ROC) curve and the area under the ROC curve (AUC) were used to check differentiation performance of all parameters only between the cervical cancer group and the healthy groups. P<0.05 was considered statistically significant.Results
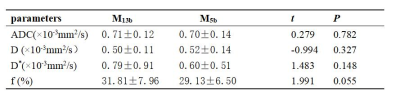
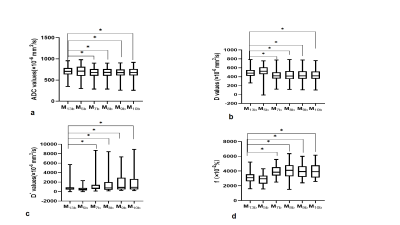
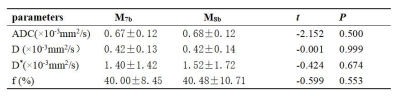
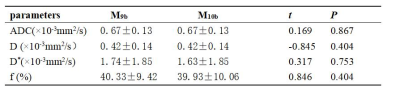
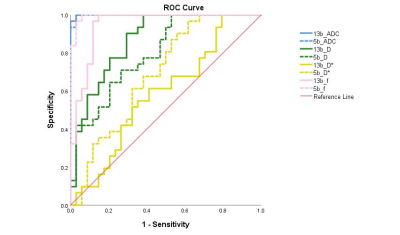
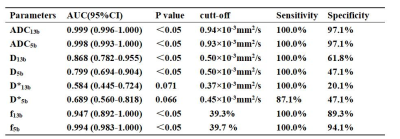
No significant difference of ADC, D, D* and f between standard 13b model (M13b) and 5b model (M5b) (P > 0.05) while between M13b and M7b, M8b, M9b as well as M10b (P < 0.05) (Table1, Figure 1). There was no statistically significant difference between M7b and M8b (P > 0.05) (Table 2) as well as between M9b and M10b (P > 0.05) (Table 3). The area under ROC curves between M13b and M5b showed high consistency, but D* failed to differentiate groups (Figure 2, Table 4).Discussion
We firstly investigated the optimal b-value protocol to build a stable IVIM model for wider clinical diagnosis in short-time, relatively real-time and at convenience. We compared the differences of ADC, D, D* and f values retrieved from 5, 7, 8, 9, 10, and 13 b values image sets using bi-exponential equation. No statistical significance of all values between M7b and M8b as well as between M9b and M10b confirmed that b values of 1000 s/mm2 and 1200 s/mm2 respectively does not affect the stability of cervical cancer model and can be removed. Abundant cervical cancer studies used 13 b-value protocol for IVIM acquisition; therefore, in our study, we used it as the standard reference model (M13b) to examine feasibility of 6 other b-value protocols. There was no significant difference of all quantitative values between M13b and M5b but M13b and the remaining b-value protocols (M7b, M8b, M9b, and M10b), possibly attributing to b value of 400 s/mm2 including in both M5b and M13b. This suggested that b value of 400 s/mm2 was the mandatory b value for cervical cancer IVIM model. Last but not the least, the ROC curves between M13b and M5b were highly consistent (P>0.05), and f value had the highest diagnostic efficiency while D* had poor diagnostic efficiency, consistent with cervical cancer studies [6, 7]. This may attribute that D* is easily influenced by b-values and visual manual measurements and the stability of D* largely relies on SNR [8, 9].Conclusions
The 5 b-value (M5b) IVIM model can replace the 13 b-value (M13b)IVIM model in the clinical diagnosis and treatment of cervical cancer, and shorten the scanning time. b=400 s/mm2 is the necessary b value for IVIM model of cervical cancer.Acknowledgements
No acknowledgement found.References
[1] Lin M, Yu X, Chen Y, et al (2017) Contribution of mono-exponential, bi-exponential and stretched exponential model-based diffusion-weighted MR imaging in the diagnosis and differentiation of uterine cervical carcinoma. Eur Radiol 27(6):2400-2410. doi: 10.1007/s00330-016-4596-8.
[2] Li X, Wang P, Li D, et al (2018) Intravoxel incoherent motion MR imaging of early cervical carcinoma: correlation between imaging parameters and tumor-stroma ratio. Eur Radiol 28(5):1875-1883. doi: 10.1007/s00330-017-5183-3.
[3] Lin L, Xue Y, Duan Q, et al (2019) Grading meningiomas using mono-exponential, bi-exponential and stretched exponential model-based diffusion-weighted MR imaging. Clin Radiol 74(8):651.e15-651.e23. doi: 10.1016/j.crad.2019.04.007.
[4] Lemke A, Stieltjes B, Schad LR,et al (2011) Toward an optimal distribution of b values for intravoxel incoherent motion imaging. Magn Reson Imaging 29(6):766-76. doi: 10.1016/j.mri.2011.03.004.
[5] Jambor I, Merisaari H, Aronen HJ, et al (2014) Optimization of b-value distribution for biexponential diffusion-weighted MR imaging of normal prostate. J Magn Reson Imaging 39(5):1213-22. doi: 10.1002/jmri.24271.
[6] Lee EY, Yu X, Chu MM,et al. (2014) Perfusion and diffusion characteristics of cervical cancer based on intraxovel incoherent motion MR imaging-a pilot study. Eur Radiol 24(7):1506-13. doi: 10.1007/s00330-014-3160-7.
[7] Wang H, Zhu L, Li G,et al. (2020) Perfusion parameters of intravoxel incoherent motion based on tumor edge region of interest in cervical cancer: evaluation of differentiation and correlation with dynamic contrast-enhanced MRI. Acta Radiol 61(8):1087-1095. doi: 10.1177/0284185119890086.
[8] Marzi S, Piludu F, Vidiri A. (2013) Assessment of diffusion parameters by intravoxel incoherent motion MRI in head and neck squamous cell carcinoma. NMR Biomed 26(12):1806-14. doi: 10.1002/nbm.3020.[9] Andreou A, Koh DM, Collins DJ, et al. (2012) Measurement reproducibility of perfusion fraction and pseudodiffusion coefficient derived by intravoxel incoherent motion diffusion-weighted MR imaging in normal liver and metastases. Eur Radiol 23(2):428-34. doi: 10.1007/s00330-012-2604-1.
Figures