3263
Diagnostic performance of synthetic MRI and reduced filed-of-view DWI-based IVIM on cervical intraepithelial neoplasis1Department of Biomedical Engineering, Hubei University of Medicine, Hubei, China, 2GE Healthcare, Beijing, China, 3Department of Radiology,Taihe Hospital, Hubei University of Medicine, Hubei, China
Synopsis
Keywords: Uterus, Cancer
CIN III is currently reckoned as a high-risk precancerous lesion for highly-possible transformation into cervical cancers. To improve low diagnostic efficiency of traditional MRI on precancerous CIN III for its subtle changes at the cellular level, this study built a combination model with MAGiC and IVIM derived parameters. In particular, a combined model with T2 and f values showed good performance on differentiation CIN III from cervical cancer with the sensitivity, specificity and AUC of 0.0.968, 0.839, 956, and it indeed elevated diagnostic performance especially specificity. In our study, alteration of heterogeneity at the cellular level was suspected to occur as cervix gradually progresses to CIN III stage despite no obvious morphological changes on structural images.Introduction
Cervical cancer is a common malignant tumor in the female reproductive system, and the recurrence of cervical intraepithelial neoplasis (CIN) easily progresses to cervical cancer. CIN III is currently reckoned as a high-risk precancerous lesion for highly-possible transformation into cervical cancers [1]. With the advantages of simultaneously displaying conventional anatomical structure images and quantitative information, synthetic magnetic resonance imaging has been widely applied in the whole body especially tumors despite its low specificity [3-4]. In addition, intravoxel incoherent motion (IVIM) imaging displays tumor area and microcirculation [5] and has higher sensitivity and accuracy in differentiating types of cervical tumors and predicting the efficacy of tumor chemoradiotherapy [6,7]. To improve low diagnostic efficiency of traditional MRI on precancerous CIN III for its subtle changes at the cellular level, this study aims to explore the diagnostic value of relaxometry parameters combined with IVIM-derived parameters in discrimination of CIN III and cervical cancer.Materials and methods
We prospectively recruited 35 cervical cancer patients, 35 healthy volunteers and 25 patients with CIN III in our hospital from May to December 2021. All patients underwent conventional axial T1WI, T2WI, and sagittal T2WI as well as additional MAGIC sequence (TR/TE =4280/14.4,86.5 ms, FOV = 22 cm, thickness =4 mm) and IVIM sequence (TR/TE =4000/71.6ms, FOV = 22 cm, thickness =4 mm, 13b) on 1.5T MRI (Signa voyager, GE Healthcare) with 8-channel abdominal phased coil in a total of 11’12’’ scan time. T1, T2 relaxation time and PD values, pure molecular diffusion (D), pseudo-diffusion coefficient (D*) and perfusion fraction (f) were obtained from synthetic MRI and IVIM data. For the cervical cancer group, lesion sketched ROIs was performed on the largest-cross-sectional lesion of the axial plain T2 image when sagittal T2 images were used as reference and then copied to six maps double-blinded by two radiologists with at least 10 years of experience in abdominal imaging diagnosis. The areas of blood vessels, tumor bleeding and necrosis were prevented to involve in ROIs. For CIN III group, the axial plain T2 images with slightly abnormal signal or the maximum cervical plane if no obvious abnormality was chosen to draw ROIs. Three ROIs were delineated in the selected slice itself and the upper and lower slices and averaged. For the healthy volunteers, the maximum level of cervix was selected to delineate the ROIs for three times, and the average value was taken. All data were presented in mean±standard deviation (xˉ±s), and independent sample t-test or Mann-Whitney U test was used for comparison between groups according normality and equality-of-variances respectively examined by Kolmogorov-Smirnov test and Levene's-Test. Receiver operating characteristic (ROC) curve and the area under the ROC curve (AUC) were used to check differentiation performance of all parameters only between the cervical cancer group and the CINIII groups. P<0.05 was considered statistically significant.Results
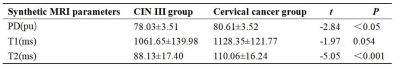
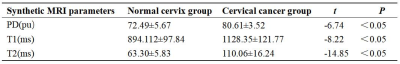
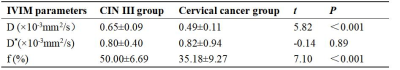
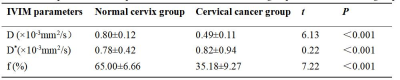
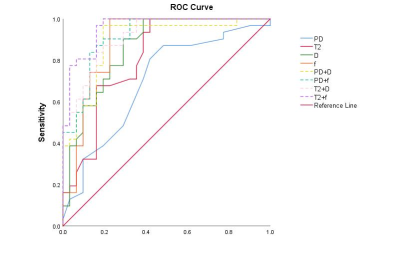
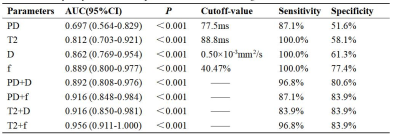
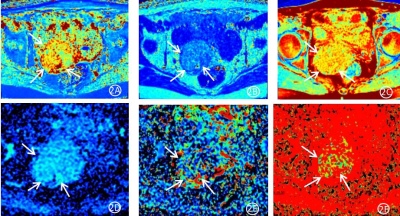
Cervical cancer group had significantly higher T2 and PD values and lower D and f values than the CIN III group and normal cervical group (P < 0.05). Significant difference of T1 and D* value was found between normal cervical group and cervical cancer group (P < 0.05) but not CINIII group (P > 0.05). All results in details were shown in Table I to Table IV. The area under the ROC curve (AUC) of T2, PD, D and f values in differentiation of cervical cancer and CIN III groups were 0.812, 0.697, 0.862, and 0.899, accordingly (P < 0.05). Based on statistically different MAGiC values (T2 and PD) and IVIM-derived values (D and f) between groups, the combination of T2 and f values showed the highest diagnostic performance with the AUC of 0.956. ROC curves of all parameters and combined models were shown in Fig. 1 and Table 5. Related pseudo-color maps generated by synthetic MRI and IVIM parameters in cervical cancer patients are shown in Figure 2.Discussion
We applied MAGiC in differentiation of CIN III patients from cervical cancer patients successfully and, of course, normal cervical group and also elevated specificity with first combining MAGiC with IVIM parameters for the model of T2 and f with the AUC of 0.956. Alteration of heterogeneity at the cellular level was suspected to occur as cervix gradually progresses to CIN III stage despite no obvious morphological changes on structural images. In our study, T1 value showed no difference between cervical cancer and CIN III groups, possibly attributing to the same precession frequency of spins in surrounding tissues returning to thermodynamic equilibrium and paralleling to the B0 direction [8]. Cervical cancer has abundant extracellular matrix and thus highly expresses Ki-67 [9], and so does CIN [10]. The more abundant extracellular matrix, the longer T1 relaxation time. Therefore, T1 values in our two patient groups were statistically longer than normal cervical group (P<0.05) and the former two groups could not be differentiated (P>0.05). Additionally, IVIM-derived D and f values in identification of CIN III from cervical cancer group fairly performed while D* performed poorly for instability and low repeatability.Conclusions
The combination model with MAGiC and IVIM derived parameters showed good performance on differentiation CIN III from cervical cancer, especially T2 and f values, and it indeed elevated diagnostic performance especially specificity.Acknowledgements
No acknowledgement found.References
[1] De Silva SS, Payne GS, Morgan VA,et al. (2009) Epithelial and stromal metabolite changes in the transition from cervical intraepithelial neoplasia to cervical cancer: an in vivo 1H magnetic resonance spectroscopic imaging study with ex vivo correlation. Eur Radiol 19(8):2041-8. doi: 10.1007/s00330-009-1363-0.
[2] Warntjes JB, Leinhard OD, West J, et al. Rapid magnetic resonance quantification on the brain: Optimization for clinical usage[J]. Magn Reson Med, 2008, 60(2):320-9.
[3] Jiang Y, Yu L, Luo X, et al. (2020) Quantitative synthetic MRI for evaluation of the lumbar intervertebral disk degeneration in patients with chronic low back pain. Eur J Radiol 124:108858. doi: 10.1016/j.ejrad.2020.108858.
[4] Zhao L, Liang M, Xie L,et al. (2021) Prediction of pathological prognostic factors of rectal cancer by relaxation maps from synthetic magnetic resonance imaging. Eur J Radiol 138:109658. doi: 10.1016/j.ejrad.2021.109658.
[5] Lin M, Yu X, Chen Y, et al. Contribution of mono-exponential, bi-exponential and stretched exponential model-based diffusion-weighted MR imaging in the diagnosis and differentiation of uterine cervical carcinoma[J]. Eur Radiol, 2017, 27(6):2400-2410.
[6] Perucho JAU, Wang M, Vardhanabhuti V, et al. Association between IVIM parameters and treatment response in locally advanced squamous cell cervical cancer treated by chemoradiotherapy[J]. Eur Radiol, 2021, 31(10):7845-7854. DOI: 10.1007/s00330-021-07817-w.
[7] Li X, Wang P, Li D, et al. Intravoxel incoherent motion MR imaging of early cervical carcinoma: correlation between imaging parameters and tumor-stroma ratio[J]. Eur Radiol, 2018, 28(5):1875-1883.[8] Kim PK, Hong YJ, Im DJ,et al. Myocardial T1 and T2 Mapping: Techniques and Clinical Applications[J]. Korean J Radiol, 2017, 18(1):113-131.
[9] Meng T, He N, He H, et al. The diagnostic performance of quantitative mapping in breast cancer patients: a preliminary study using synthetic MRI[J]. Cancer Imaging, 2020, 20(1):88.
[10] De Silva SS, Payne GS, Morgan VA, et al. Epithelial and stromal metabolite changes in the transition from cervical intraepithelial neoplasia to cervical cancer: an in vivo 1H magnetic resonance spectroscopic imaging study with ex vivo correlation[J]. Eur Radiol, 2009, 19(8):2041-8. DOI: 10.1007/s00330-009-1363-0.
Figures