3260
Diffusion kurtosis imaging with multiple quantitative parameters for predicting microsatellite instability status of endometrial carcinoma
Qingling Song1, Wan Dong2, Shifeng Tian3, Lihua Chen3, and Ailian Liu3
1Radiology, the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Radiology, Wuhan children's Hospital, Tongji Medical College of Huazhong University of Science & Technology, Wuhan, China, 3Radiology, The First Affiliated Hospital of Dalian Medical University, Dalian, China
1Radiology, the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Radiology, Wuhan children's Hospital, Tongji Medical College of Huazhong University of Science & Technology, Wuhan, China, 3Radiology, The First Affiliated Hospital of Dalian Medical University, Dalian, China
Synopsis
Keywords: Pelvis, Cancer
Microsatellite instability (MSI), which results from the failure of mismatch repair (MMR) proteins to fix a DNA replication error, causes insertions, mismatches, or deletions during the DNA replication process, thus having an essential role in maintaining the stability of the genome and regulating gene expressionSynopsis
Microsatellite instability (MSI), which results from the failure of mismatch repair (MMR) proteins to fix a DNA replication error, causes insertions, mismatches, or deletions during the DNA replication process, thus having an essential role in maintaining the stability of the genome and regulating gene expressionSummary of main Findings
This study showed that the MK and Ka values of the MSI group were higher than those of the MSS group (P<0.05), and the MD and Dr values were lower than those of the MSS groupIntroduction and Purpose
Microsatellite instability (MSI), which results from the failure of mismatch repair (MMR) proteins to fix a DNA replication error, causes insertions, mismatches, or deletions during the DNA replication process, thus having an essential role in maintaining the stability of the genome and regulating gene expression (1-3). MSI is considered as one of the pathogenesis of endometrial carcinoma (EC) (4). The use of magnetic resonance imaging (MRI) related techniques can be used to predict the MSI status of EC before surgery. The diffusion kurtosis imaging (DKI) sequence is an extension of the diffusion-weighted imaging (DWI) and the diffusion tensor imaging (DTI) sequence. This study aimed to explore the value of multiple quantitative parameters of DKI sequence in predicting MSI status of EC to provide new ideas for non-invasive preoperative diagnosis in predicting MSI status and expanding the application of DKI sequence for uterine diseases.Materials and Methods
38 patients were collected in the study, including 12 in the MSI group and 26 in the MSS group. MR examinations included T1W, T2W and DKI were performed within two weeks before surgery. The specific scanning parameters are shown in Table 1. Referring to the T2WI images, the largest section of the lesion and it's upper and lower 1-2 levels were selected. The regions of interest (ROIs) were manually drawn in the tumor parenchymal area, avoiding the areas of necrosis, hemorrhage, and cystic degeneration, and appropriately avoiding the lesion's edge, after which the average value was taken. The quantitative parameters included mean kurtosis (MK), axial kurtosis (Ka), radial kurtosis (Kr), and fractional anisotropy (FA), fractional anisotropy of kurtosis (FAk), mean diffusivity (MD), axial diffusivity (Da), and radial diffusivity (Dr) (Figure 1). The independent-sample t-test (normal distribution) or Mann-Whitney U test (skew distribution) was used to compare the differences between the parameter values of the two groups. The receiver operator characteristic (ROC) curve was used to analyze the diagnostic efficiency and the best diagnostic threshold of different parameters. The area under curve (AUC) was calculated, as well as the corresponding sensitivity and specificity.Results
Patient Characteristics Patients in the MSI group were 47-82 years old, with an average of (64.1±9.8) years old; there were 2 premenopausal cases and 10 post-menopausal cases. Patients in the MSS group were 35-78 years old, with an average of (56.7±12.8) years old; there were 12 cases before menopause and 14 cases after menopause. Agreement on Imaging Parameters among the Three Observers The consistency test results of the parameters between the two groups by the two observers are shown in Table 2, and the consistency of the data in each group was very good (ICC>0.75). Comparison of DKI parameters between the two groups The parameter values and results comparison between the MSI group and the MSS group are shown in Table 3. The MD and Dr values of the MSI group were smaller than those in the MSS group, while the MK and Ka values were greater than those in the MSS group. The differences were statistically significant. Efficacy of various parameters to diagnose MSI of EC and their comparison results The parameters of the DKI sequence to identify the AUC of the two groups, the threshold, sensitivity and specificity of predicting MSI status of EC are shown in Table 4; the ROC curve is presented in Figure 2.Discussion and Conclusion
MSI is closely related to the occurrence of Lynch syndrome (LS). Patients with LS have a significantly increased risk of developing colorectal cancer, ovarian cancer, and EC. EC usually occurs before other tumors and is considered the "sentinel Cancer" of LS patients. (5,6). Our results showed that the MK and Ka values of EC in the MSI group (1.074±0.162, 1.253±0.229) were higher than those in the MSS group (0.956 (0.889,1.002), 1.048±0.211). MD and Dr values in the MSI group were lower than those of the MSS group. As the activity and ability of tumor cell proliferation of MSI-related EC are higher than that of MSS-related EC, and there are more lymphocytes and other substances infiltrating tumor tissue, it is speculated that the tumor cells of MSI-related EC are more compactly arranged, the extracellular space is smaller, and the degree of water molecule diffusion is more restricted. In conclusion, as non-enhanced functional imaging of MR, DKI can provide multiple quantitative parameters for non-invasive prediction of MSI status of EC, such as MK, Ka, MD, and Dr, and it has certain clinical application value.Acknowledgements
no acknowledgementsReferences
References 1. Tamura K, Kaneda M, Futagawa M, et al. Genetic and genomic basis of the mismatch repair system involved in Lynch syndrome. Int J Clin Oncol 2019; 24:999-1011. 2. Kane AM, Fennell LJ, Liu C, et al. Alterations in signaling pathways that accompany spontaneous transition to malignancy in a mouse model of BRAF mutant microsatellite stable colorectal cancer. Neoplasia 2020;22:120-128. 3. Greenberg A, Kariv R, Solar I, et al. Geographic Heterogeneity for Mismatch Repair Proteins Is Associated with Defects in DNA Repair. Isr Med Assoc J 2020; 22:32-36. 4. Brooks RA, Fleming GF, Lastra RR, et al. Current recommendations and recent progress in endometrial cancer. CA Cancer J Clin 2019; 69:258-279. 5. Ryan N, Wall J, Crosbie EJ, et al. Lynch syndrome screening in gynaecological cancers: results of an international survey with recommendations for uniform reporting terminology for mismatch repair immunohistochemistry results. Histopathology 2019; 75:813-824. 6. Kahn RM, Gordhandas S, Maddy BP, et al. Universal endometrial cancer tumor typing: How much has immunohistochemistry, microsatellite instability, and MLH1 methylation improved the diagnosis of Lynch syndrome across the population? Cancer 2019; 125:3172-3183.Figures
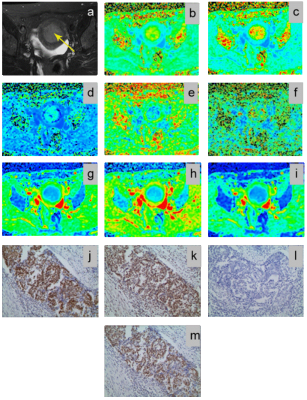
Fig. 1. A 51-year-old patient with poorly differentiated
EC. a, The lesion is showed on T2WI
(yellow arrow). b-i, The
pseudo-color images of MK, Ka, Kr, FA, FAk, MD, Da, and Dr of the DKI sequence.
Their quantitative values are 1.295, 1.525, 1.115, 0.168, 0.355, 0.673 μm2/ms,
0.786 μm2/ms and 0.616 μm2/ms, respectively. j~m, Immunohistochemical staining,
showing strong staining of MLH-1 (j), strong staining of MSH-2 (k), loss of
expression of MSH-6 (l), strong staining of PMS-2 (m).
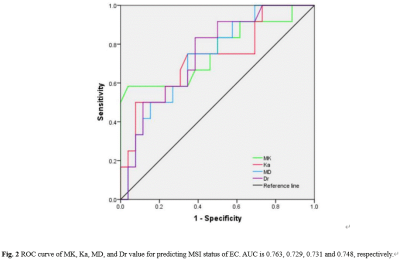
Fig. 2 ROC curve of MK, Ka, MD,
and Dr value for predicting MSI status of EC. AUC is 0.763, 0.729, 0.731 and
0.748, respectively.
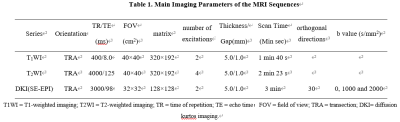
Table 1. Main Imaging Parameters of the MRI
Sequences
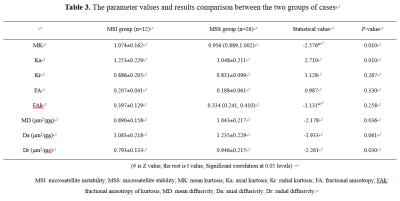
Table 3. The parameter
values and results comparison between the two groups of cases
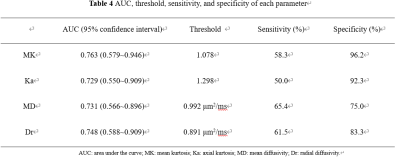
Table
4 AUC, threshold, sensitivity, and
specificity of each parameter
DOI: https://doi.org/10.58530/2023/3260