3258
Evaluation of lymphovascular space invasion in endometrial carcinoma by APTw and mDIXON-Quant1Department of Radiology, the First Affiliated Hospital of Dalian Medical University, Dalian, China
Synopsis
Keywords: Uterus, Cancer
Lymphovascular space invasion(LVSI)is one of the important factors for poor prognosis of endometrial carcinoma(EC).Quantitative parameters of amide proton transfer weighted(APTw)and Modified Dixon quantification of fat(mDIXON-Quant) is a novel MRI tool to evaluating LVSI in EC. The APT and R2* values of LVSI(+)EC were higher than those of LVSI(-)EC.APT value was moderately positively correlated with R2* value, and APT value was weakly positively correlated with FF value . Both APTw and Mdixon-Quant techniques can effectively evaluate EC LVSI, and their combined application can improve the evaluation efficiency.Objective
To investigate the amide proton transfer weighted (APTw) and Modified Dixon quantification of fat. Value of mdixon-Quant technique in the assessment of lymphovascular space invasion (LVSI) in endometrial carcinoma (EC).Materials and Methods
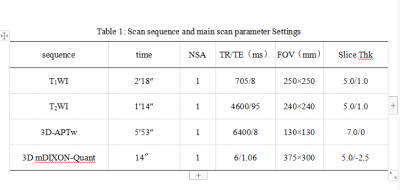
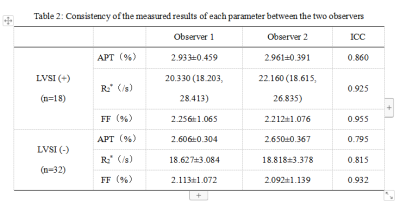
The data of 50 EC patients confirmed by surgery and pathology were retrospectively analyzed, including 18 patients with LVSI(LVSI(+) and 32 patients without LVSI(LVSI(-). Preoperative MR scan sequences included APTw and Mdixon-Quant. APT, transverse relaxation rate (R2*) and fat fraction (FF) plots were obtained by postprocessing. The APT, R2* and FF values of the two groups of cases were measured by two observers, and the consistency of the measurement results of each parameter value between the two observers was tested by intra-class correlation coefficients (ICC). The independent sample t-test or Mann-Whitney U test was used to compare the differences of parameters between the two groups. Receiver operating characteristic curve was used to evaluate the statistically significant parameters and the efficacy of LVSI after combined evaluation. Delong test was used to compare the differences between the area under curve (AUC) of each curve, and Pearson correlation analysis was used to evaluate the correlation between APT value and R2* and FF value.Results
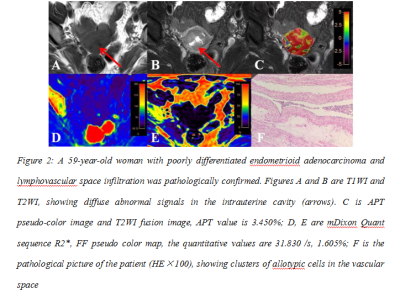
The agreement between the two observers was good (ICC>0.75). The APT, R2* and FF values of LVSI(+)EC were 2.947±0.399 %, 20.605 (18.525, 27.953) /s and 2.234±1.047 %, respectively. The above parameters of LVSI(-)EC were 2.628±0.307 %, 18.968 (16.225, 20.544) /s and 2.103±1.070 %, respectively. The APT and R2* values of LVSI(+)EC were higher than those of LVSI(-)EC (P<0.05). There was no difference in FF value between the two groups (P>0.05). The AUC values of APT, R2* and APT+R2* for LVSI were 0.751, 0.713 and 0.781, respectively, and there was no significant difference among the AUC values (P>0.05). APT value was moderately positively correlated with R2* value (r=0.528, P<0.001), and APT value was weakly positively correlated with FF value (r=0.312, P=0.027).Conclusion
Both APTw and Mdixon-Quant techniques can effectively evaluate EC LVSI, and their combined application can improve the evaluation efficiency.Acknowledgements
noneReferences
[1] Stålberg K, Bjurberg M, Borgfeldt C, et al. Lymphovascular space invasion as a predictive factor for lymph node metastases and survival in endometrioid endometrial cancer - a Swedish Gynecologic Cancer Group (SweGCG) study. Acta Oncol, 2019, 58(11):1628-1633.
[2] Raffone A, Travaglino A, Raimondo D, et al. Lymphovascular space invasion in endometrial carcinoma: A prognostic factor independent from molecular signature. Gynecol Oncol. 2022 Apr;165(1):192-197. doi: 10.1016/j.ygyno.2022.01.013.
[3] Harris KL, Maurer KA, Jarboe E, et al. LVSI positive and NX in early endometrial cancer: Surgical restaging (and no further treatment if N0), or adjuvant ERT? Gynecol Oncol, 2020, 156(1):243-250.
[4] Ironi G, Mapelli P, Bergamini A, et al. Hybrid PET/MRI in Staging Endometrial Cancer: Diagnostic and Predictive Value in a Prospective Cohort. Clin Nucl Med, 2022, 47(3):e221-e229.
[5] Colombo N, Creutzberg C, Amant F, et al. ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: Diagnosis, Treatment and Follow-up. Int J Gynecol Cancer, 2016, 26(1):2-30.
Figures