3251
MAVRIC SL can reduce inter-rater variability of the measurements for the cervical spine segment height in ACDF patients on 3T MRI1Renmin Hospital of Wuhan University, Wuhan, China, 2GE Healthcare, Beijing, China
Synopsis
Keywords: Artifacts, Surgery
Subsidence assessment is an important indicator for postoperative follow-ups for ACDF patients and normally performed on radiographs. It is still challenging to image ACDF patients using conventional MRI for the measure of segment height is influenced by the metal artifacts. In this study, MAVRIC SL showed better inter-rater agreement on measurements of segment height compared to FSE T1WI. 20 cases on MAVRIC SL and 6 cases on FSE T1W1 among 22 patients showed the measurements of segment height was less than the maximum allowed difference (2mm). This study demonstrated that MAVRIC SL has a strong potential in the subsidence assessment.Background
Anterior cervical discectomy and fusion (ACDF) procedure has been widely used for central and foraminal decompression in various cervical pathologies.1, 2 Imaging assessment of cage subsidence is an important indicator for postoperative follow-ups for the ACDF patients. To assess the cage subsidence, the segment height is commonly measured on the X-ray images depending on visibility of the endplates.3 However, the visibility of the endplates is susceptible to the metal artifacts on the standard MRI. Multi-acquisition with variable resonance image combination slab selectivity (MAVRIC SL) applies multiple RF spectral bins and additional complementary gradients to achieve metal artifact suppression, bringing benefits to image large metal implants in arthroplasty.4-6 In this study, we explore the feasibility of that MAVRIC SL sequence can reduce the metal artifacts and makes for measurement of the segment height compared to the standard MRI sequences.Methods
Patients: 22 ACDF patients (12 men; mean age = 48.0 ± 15.8 years) were involved in this study. The time intervals between the MRI examination and the surgery for these patients ranged from 7 days to 2 years. ACDF surgeries included 1 level in 7 cases, 2 levels in 12 cases, and 3 levels in 3 cases. Image acquisition: All MR images were acquired on a 3.0 T MR scanner (Discovery 750w; GE Medical Systems, Milwaukee, WI, USA). Imaging sequences included the standard FSE sequences (sagittal FSE T2WI, T1WI and axial FSE T2WI) and sagittal MAVRIC SL sequence. Image analysis: On the paired mid-sagittal planes of the FSE T1W and MAVRIC SL images, metal artifact areas were delineated by one musculoskeletal radiologist, and the segment heights were measured by two musculoskeletal radiologists independently. Statistical Analysis: The overall metal artifact area between the FSE T1WI and MAVRIC SL images were compared with a paired Student t-test or Wilcoxon signed test according to data normality and equality of variance. To investigate inter-rater variability of the measurement of the segment heights, bias (mean difference), limits of agreement values (LoA) and the percentage of the cases that exceeded the maximum allowed difference were calculated using a Bland and Altman analysis. Referring to the subsidence evaluation criteria,7 the maximum allowed difference was specified as 2 mm.Results
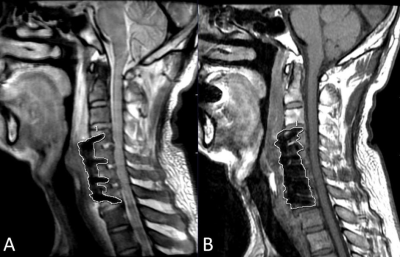
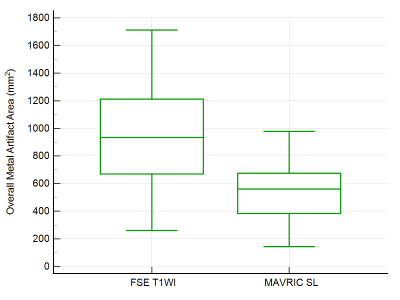
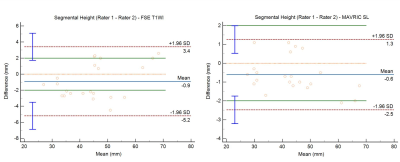
The overall metal artifact area for the MAVRIC SL and FSE T1WI sequences were 526 ± 203 mm2 and 905 ± 358 mm2, respectively. Compared to FSE T1WI, the overall area of metal artifacts was significantly reduced by 42% (t = 10.537, P < 0.001) (Fig. 1 and Fig. 2). With respect to the inter-rater variability for the measurements of the segment height, Bland-Altman analysis revealed a bias of -0.6 mm (ranging from -2.1 mm to 1.1 mm; LoA: -2.5 mm, 1.3 mm) for MAVRIC SL and a bias of -0.9 mm (ranging from -4.5 mm to 2.6 mm; LoA: -5.2 mm, 3.4 mm) for FSE T1WI. There were 27% (6/22) of cases that were less than the maximum allowed difference for FSE T1WI compared to 91% (20/22) of those for MAVRIC SL (Fig. 3).Discussion
This study demonstrated that the metal artifacts on the MAVRIC SL images were significantly suppressed compared to the bandwidth-optimized FSE T1WI sequence, contributing to more reliable measurements of the segment height. To determine the restoration in the height of the neural foramens, subsidence is routinely assessed and defined as a decrease of more than 2 mm in the segment heights between the final follow-up and immediate post-surgery examination.7 Therefore, the reliability of the subsidence assessment was highly affected by metal artifact on MRI. It is accepted that T1W and PDW FSE sequences with relatively shorter TE showed smaller artifacts than T2W sequences with longer TE.8 However, the endplates within the fused segment on the FSE T1WI images overlaid with metal artifacts and there were only 27% of the inter-rater measurement bias less than 2 mm, leading to an incorrect subsidence assessment. In contrast, the area of metal artifacts was significantly reduced on the MAVRIC SL images and there were 91% of the inter-rater measurement bias less than 2 mm. Our study showed MAVRIC SL with the features of the multi-acquisition with variable resonance image combination (MAVRIC), slice-encoding for metal artifact correction (SEMAC), and view angle tilting (VAT) to resolve through-plane and in-plane artifact successfully achieve metal artifact suppression in patients with ACDF.4 Although X-ray is a routine method for the subsidence assessment, we did not compare both modality for the inconsistencies of cervical curvature and gravity in the long axis caused by different patient positions between MRI and X-ray.Conclusion
MAVRIC SL sequence can significantly reduce the metal artifacts of cervical spine MRI for the ACDF patients compared to the standard FSE T1WI sequence, showing a great potential in subsidence assessment of long-term tracking patients with ACDF.Acknowledgements
No acknowledgement found.References
1. Hirvonen T, Siironen J, Marjamaa J, et al. Anterior cervical discectomy and fusion in young adults leads to favorable outcome in long-term follow-up[J]. The Spine Journal,2020,20(7):1073-1084.
2. Findlay C, Ayis S, Demetriades A K. Total disc replacement versus anterior cervical discectomy and fusion[J]. The Bone & Joint Journal,2018,100-B(8):991-1001.
3. Kani K K, Chew F S. Anterior cervical discectomy and fusion: review and update for radiologists[J]. Skeletal Radiology,2018,47(1):7-17.
4. Gutierrez L B, Do B H, Gold G E, et al. MR Imaging Near Metallic Implants Using MAVRIC SL[J]. Academic Radiology,2015,22(3):370-379.
5. Choi S, Koch K M, Hargreaves B A, et al. Metal Artifact Reduction With MAVRIC SL at 3-T MRI in Patients With Hip Arthroplasty[J]. American Journal of Roentgenology,2015,204(1):140-147.
6. Kretzschmar M, Nardo L, Han M M, et al. Metal artefact suppression at 3 T MRI: comparison of MAVRIC-SL with conventional fast spin echo sequences in patients with Hip joint arthroplasty[J]. European Radiology,2015,25(8):2403-2411.
7. Moo I H, Kam C J W, Lai M W S, et al. A comparison of contiguous two-level anterior cervical discectomy and fusion using a structural allograft versus a Polyetheretherketone (PEEK) cage: the results of a three-year follow-up[J]. BMC Musculoskeletal Disorders,2020,21(1).
8. Harris C A, White L M. Metal Artifact Reduction in Musculoskeletal Magnetic Resonance Imaging[J]. Orthopedic Clinics of North America,2006,37(3):349-359.
Figures