3232
Discussion the WHO grading of brain invasion otherwise benign meningiomas (BIOB) from the MR images perspective of 675 meningiomas1Medical Imaging Department, Shenzhen The Second People's Hospital, Shenzhen, China, 2Zhuhai People’s Hospital (Zhuhai hospital affiliated with Jinan University), Zhuhai, China, 3Philips Healthcare, Guangzhou, China
Synopsis
Keywords: Tumors, PET/MR, WHO grade
Should the BIOB meningiomas be classified as WHO grade 1 or WHO grade 2 atypical meningiomas, the core issue that scholars have questioned about the guidelines from an imaging perspective.In this study, we used BIOB as the entry point to comprehensively compare and analyze the MRI imaging characteristics of BIOB between WHO grade 1 and 2 meningiomas. Comparative analysis of multiple groups of MRI characteristics showed that BIOB and WHO grade 2 meningiomas were more similar in clinical and imaging features than grade 1 meningiomas. Therefore, it is reasonable to classify BIOB as WHO grade 2 meningiomas in the guidelines.Introduction
The World Health Organization (WHO) has classified the meningiomas into three grades. Tumor grading can influence considerations about patients’ prognosis, treatment options and response to therapy. However, brain invasion otherwise benign (BIOB) meningiomas should be classified as WHO grade 1 or WHO grade 2 atypical meningiomas is still a controversial issue. Thus, in this study, we aimed to compare and analyze the MRI imaging features of BIOB meningiomas with WHO grade 1 as well as grade 2 meningiomas, and discuss the WHO grading of BIOB from the perspective of imaging.Materials and Methods
A retrospective analysis was performed on 675 meningioma patients who underwent MRI examinations including T1WI, T2WI,DWI and contrast-enhanced T1WI (CE-T1WI) from January 2006 to February 2022. Two senior neuroradiologists(11 years/16 years working experience) who blinded to the pathological findings analyzed the conventional MRI characteristics according to the 2022 edition of the WHO guidelines. For the ADC analysis, the slice with the maximum lesion was selected and five 5-mm-diameter ROIs were placed on the sloid portion of the tumor.The average ADC value of five ROIs was calculated. Finally, a total of 17 features were obtained. The 2022 Central nervous system (CNS) WHO Guidelines were set as the gold standard for pathological diagnosis. The univariate logistic regression was performed to determine the independent risk factors for identifying BIOB and WHO grade 1 meningiomas. And then the significant factors were further selected for multivariate logistic regression analysis.The same statistical method was used for identifying BIOB and WHO grade 2 meningiomas too.The diagnostic efficacy was analyzed using the receiver operator characteristic curve (ROC),and the area under the curve (AUC), sensitivity and specificity were calculated.The statistical analysis was performed with SPSS version 26.0 software, and a p value < 0.05 was considered statistically significant.Results
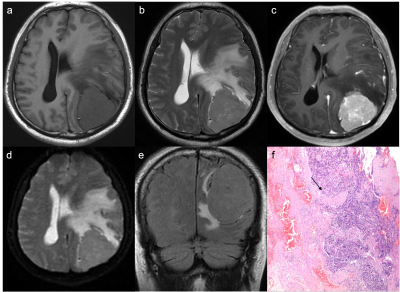
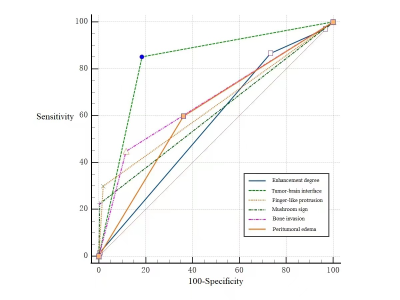
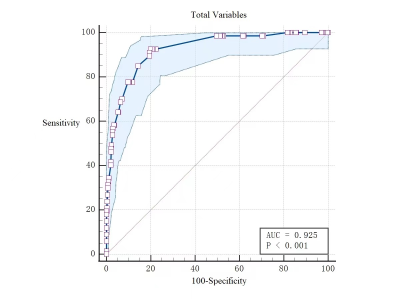
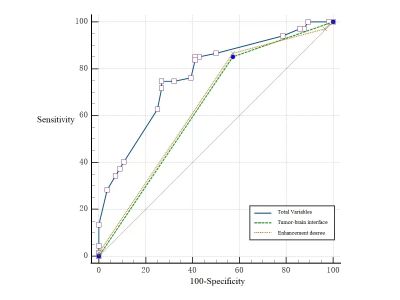
Among 675 patients with meningiomas, 543 (80.4%) were WHO grade 1, 123 (18.2%) were WHO grade 2, and 9 (1.3%) were WHO grade 3. There were 108 patients with meningiomas with brain invasion (BI) (16.0%) and 567 patients without BI (84.0%). Among the BI patients, 67 patients were BIOB. Comparing the MRI features between the BIOB and WHO grade 1 meningiomas, the multivariate analysis showed that the significant factors were enhancement degree, peritumoral edema, tumor-brain interface, fingerlike protrusion, mushroom sign and bone invasion (AUC: 0.925 (0.901~0.945), sensitivity: 92.5%, specificity:80.1%). Comparing the MRI features between the BIOB and WHO grade 2 meningiomas, the multivariate analysis demonstrated that the significant factors were enhancement degree and the tumor-brain interface (AUC: 0.779 (0.686~0.841), sensitivity: 74.6%, specificity: 73.2%).Conclusions
BIOB is more similar to WHO grade 2 meningiomas in clinical and imaging features than WHO grade 1, so it is reasonable to classify BIOB as grade 2 meningiomas in the guidelines.Acknowledgements
No acknowledgement found.References
1. Hammouche S, Clark S, Wong A, Eldridge P, Farah J. Long-term survival analysis of atypical meningiomas: survival rates, prognostic factors, operative and radiotherapy treatment. Acta neurochirurgica 2014;156(8):1475-1481.
2. Wang YC, Chuang CC, Wei KC, et al. Long Term Surgical Outcome and Prognostic Factors of Atypical and Malignant Meningiomas. Sci Rep 2016;6:35743.
3.Nakasu S, Nakasu Y. Prognostic significance of brain invasion in meningiomas: systematic review and meta-analysis. Brain Tumor Pathol 2021;38(2):81-95.
4. Perry JR, Tucker WS, Chui M, Bilbao JM. Dural cavernous hemangioma: an under-recognized lesion mimicking meningioma. Can J Neurol Sci 1993;20(3):230-233.
5. Perry A, Stafford SL, Scheithauer BW, Suman VJ, Lohse CM. Meningioma grading: an analysis of histologic parameters. Am J Surg Pathol 1997;21(12):1455-1465.
6.von Spreckelsen N, Kesseler C, Brokinkel B, Goldbrunner R, Perry A, Mawrin C. Molecular neuropathology of brain-invasive meningiomas. Brain Pathol 2022;32(2):e13048, DOI: 10.1111/bpa.13048.
7.Kandemirli SG, Chopra S, Priya S, et al. Presurgical detection of brain invasion status in meningiomas based on first-order histogram based texture analysis of contrast enhanced imaging. Clin Neurol Neurosurg 2020;198:106205, DIO:10.1016/j.clineuro.2020.106205.
Figures