3227
Identification of a single-dose, low-flip angle based CBV threshold for fractional tumor burden (FTB) mapping in recurrent glioblastoma
Aliya Anil1, Ashley M Stokes1, Lea Alhilali2, John P Karis2, Laura C Bell3, Leland S Hu4, Jerrold L Boxerman5, Kathleen M Schmainda6, and C Chad Quarles7
1Division of Neuroimaging Research and Barrow Neuroimaging Innovation Center, Barrow Neurological Institute, Phoenix, AZ, United States, 2Neuroradiology, Southwest Neuroimaging at Barrow Neurological Institute, Phoenix, AZ, United States, 3Early Clinical Development, Genentech, San Francisco, CA, United States, 4Department of Radiology, Division of Neuroradiology, Mayo Clinic Arizona, Phoenix, AZ, United States, 5Department of Neuroradiology, Rhode Island Hospital, Providence, RI, United States, 6Department of Biophysics, Medical College of Wisconsin, Milwaukee, WI, United States, 7The University of Texas MD Anderson Cancer Center, Houston, TX, United States
1Division of Neuroimaging Research and Barrow Neuroimaging Innovation Center, Barrow Neurological Institute, Phoenix, AZ, United States, 2Neuroradiology, Southwest Neuroimaging at Barrow Neurological Institute, Phoenix, AZ, United States, 3Early Clinical Development, Genentech, San Francisco, CA, United States, 4Department of Radiology, Division of Neuroradiology, Mayo Clinic Arizona, Phoenix, AZ, United States, 5Department of Neuroradiology, Rhode Island Hospital, Providence, RI, United States, 6Department of Biophysics, Medical College of Wisconsin, Milwaukee, WI, United States, 7The University of Texas MD Anderson Cancer Center, Houston, TX, United States
Synopsis
Keywords: Tumors, DSC & DCE Perfusion
Early differentiation of tumor recurrence from post treatment radiation effects (PTRE) in glioblastoma patients would improve patient management. The purpose of this study is to identify the optimal standardized relative cerebral blood volume (sRCBV) threshold for generating fractional tumor burden (FTB) maps derived from the new consensus protocol, single-dose, low-flip angle data. To establish the threshold, low-flip angle data was compared to well-validated, double-dose, moderate-flip angle data. In summary, with the optimized threshold, the single-dose, low-flip angle approach yielded FTB maps that strongly agreed with the reference standard, providing a compelling option for clinical use.
Introduction
Dynamic susceptibility contrast (DSC) MRI derived relative cerebral blood volume (rCBV) is often used for the differentiation of tumor recurrence from post-treatment radiation effects (PTRE) in glioblastoma patients. Image-guided histopathology and spatially matched DSC-MRI have identified rCBV threshold that separates PTRE from tumor recurrence1. Application of rCBV thresholds yields maps that quantify the fraction of tumor voxels relative to PTRE voxels, a biomarker termed fractional tumor burden (FTB) metric.FTB is generally measured using the double-dose, moderate flip-angle DSC-MRI acquisition protocol data with histologically validated rCBV threshold. Recently, studies have reported that single-dose, low-flip angle (LFA) CBV data agrees with the double-dose, moderate-flip angle (MFA) CBV data and thus was adopted as a new consensus protocol for imaging glioblastoma patients3,4. In this study, we identify the sRCBV threshold for the single-dose, low-flip angle DSC-MRI approach to generate FTB maps that distinguish tumor from PTRE.
Methods
This study included a cohort of 74 glioblastoma patients undergoing perfusion scans to confirm suspected tumor recurrence. Low-flip angle and moderate-flip angle DSC-MRI perfusion data were acquired during two sequential contrast agent injections. Scan parameters for the single-dose, LFA scan were TR= 1.5s, TE = 30ms, flip angle = 30º. The double-dose, MFA scan parameters matched recent recommendations3.For each patient, standardized rCBV (sRCBV) maps were generated for both the protocols using the FDA-approved clinical software, IB Neuro™, and registered to the post-contrast T1-weighted images using IB Delta Suite™. To assess sRCBV agreement between acquisition protocols, the concordance correlation coefficient (CCC) was computed between the mean tumor sRCBV values across all patients. The reference FTB map was computed from the double-dose MFA protocol data using sRCBV thresholds of 1.0 and 1.75, which defines three categories: PTRE (sRCBV < 1.0), tumor voxels with moderate angiogenesis (sRCBV: 1.0 - 1.75), and tumor voxels with high angiogenesis (sRCBV > 1.75)2. A receiver operating characteristic (ROC) analysis was performed in MATLAB to identify the optimum single-dose, low-flip angle sRCBV threshold corresponding to the maximum value of accuracy to create FTB maps that best match with the reference double-dose, moderate flip-angle FTB maps. The sensitivity, specificity and accuracy were compared between the obtained and standard reference thresholds.
Results/Discussion
Figure 1 shows the mean sRCBV correlation between the single-dose, LFA data and the corresponding double-dose, MFA data. Consistent with the prior study4, there is strong agreement in sRCBV between the two protocols (CCC = 0.98). Figure 2 shows the ROC curves that indicate a maximum accuracy for sRCBV thresholds of 1.0 (differentiating tumor vs PTRE) and 1.51 (differentiating tumor with moderate angiogenesis vs tumor with high angiogenesis). The sensitivity, specificity and accuracy corresponding to these thresholds are as follows: 87.96%, 89.90% and 88.93% for sRCBV threshold of 1.0, and 89.74%, 90.42% and 90.08% for sRCBV threshold of 1.51, respectively. Figure 3 visually summarizes several cases showing post-contrast T1-weighted images and the corresponding FTB maps for both protocols. The two protocols provide spatially similar FTB maps, supporting their similar clinical utility.Conclusion
While the prior study4 validated agreement of mean sRCBV values between the protocols, this study confirmed the spatial agreement between the tumor and PTRE using FTB mapping. The low-flip angle approach enables lower contrast agent dose, improved reproducibility by mitigating variations in preload dose and incubation time, and robust rCBV and FTB mapping.Acknowledgements
NIH/NCI 1R01CA264992-01, U01 CA176110, R01 CA255123References
- L.S. Hu, J.M. Eschbacher, J.E. Heiserman. Reevaluating the imaging definition of tumor progression: perfusion MRI quantifies recurrent glioblastoma tumor fraction, pseudoprogression, and radiation necrosis to predict survival. Neuro-Oncol. 2012; 14(7): 919-30.
- J.M. Hoxworth, J.M. Eschbacher, A.C. Gonzales. Performance of standardized relative CBV for quantifying regional histologic tumor burden in recurrent high-grade glioma: Comparison against normalized relative CBV using image-localized stereotactic biopsies. AJNR 2020; 41(3): 408-415.
- J.L. Boxerman, C.C. Quarles, L.S. Hu. Consensus recommendations for a dynamic susceptibility contrast MRI protocol for use in high-grade gliomas. Neuro-Oncol, 2020; 22(9): 1262-1275.
- K.M. Schmainda, M.A. Prah, L.S. Hu. Moving toward a consensus DSC-MRI protocol: Validation of low-flip angle single-dose option as a reference standard for brain tumors. AJNR 2019; 40(4): 626-33.
Figures
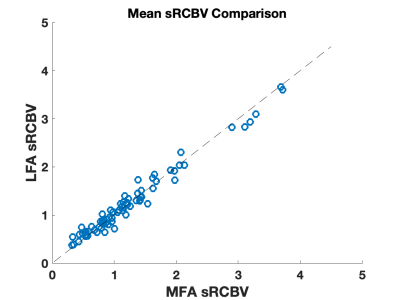
A comparison of mean tumor sRCBV values from single-dose, low-flip angle data and double-dose, moderate-flip angle across all patients included in the study. The concordance correlation coefficient across this patient cohort was 0.98.
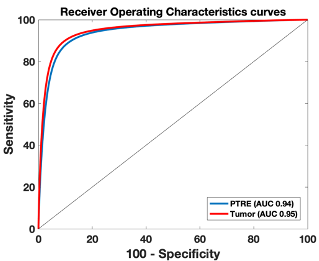
Receiver Operating Characteristics curve for the tumor and PTRE. The AUROC for tumor and PTRE are 0.94 and 0.95, respectively.
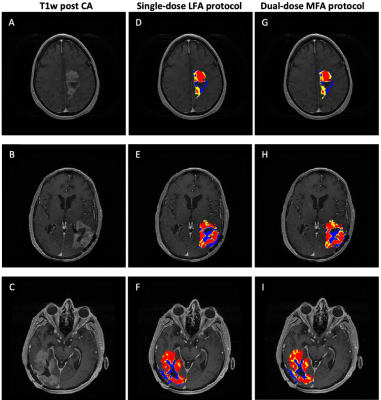
FTB map generated for the LFA and MFA protocols. (A-C): Anatomical post-contrast T1-weighted images. (D-F): FTB maps generated for the single-dose, LFA protocol. (G-I): Reference FTB maps generated for the double-dose, MFA protocol. Blue represents corresponds to PTRE (sRCBV < 1.0); yellow and red regions correspond to tumor regions (sRCBV > 1.0) with moderate and high angiogenesis, respectively.
DOI: https://doi.org/10.58530/2023/3227