3121
Habitats Analysis in Hepatocellular Carcinoma to Predict Microvascular Invasion by Intravoxel Incoherent Motion: A Pilot Study
Chenhui Li1, Jinhuan Xie1, Liling Long1, Huiting Zhang2, and Yang Song2
1The First Affiliated Hospital of Guangxi Medical University, Nanning, China, 2MR Scientific Marketing, Siemens Healthineers, Shanghai, China
1The First Affiliated Hospital of Guangxi Medical University, Nanning, China, 2MR Scientific Marketing, Siemens Healthineers, Shanghai, China
Synopsis
Keywords: Data Analysis, Segmentation, Habitats
The method of delineating the ROI of whole lesions on quantitative parameter images and then averaging them for comparison did not accurately quantify heterogeneity. In this study, we adopted a habitats analysis method combined with tissue cellularity and blood flow information from IVIM model to segment whole tumor to four subregions to predict microvascular invasion (MVI) in hepatocellular carcinoma. The results show that habitats analysis predicts MVI positivity with an accuracy of 70.19%, and the averaged value of each parameter in whole tumor was not predictive for MVI. This provides a good starting point for further application of this method.Introduction
Recently, intravoxel incoherent motion(IVIM) diffusion-weighted imaging has been used to identify pathological features of hepatocellular carcinoma(HCC), such as positive MVI 1. However, due to the heterogeneity of the tumor, in addition to the different ways of defining ROI (2D or 3D, including or excluding necrotic fractions, etc.), the extraction method of quantitative parameters (taking the average or histogram information) is also an important reason for the accuracy and consistency of the results. Tumor heterogeneity may influence imaging parameters of the whole volume analysis. Therefore, the method of delineating the ROI of the whole lesion and taking the average of quantitative parameter for comparison is not a good quantification of these heterogeneities, and accuracy and repeatability are also reduced. In recent years, habitat analysis has been increasingly used with increased temporal and spatial resolution, and has been shown to improve the quantitative assessment of tumor heterogeneity by MRI2. Therefore, the purpose of this study was to investigate whether IVIM combined with habitat analysis methods can more accurately predict microvascular invasion (MVI) HCC compared with the average value of the whole lesion ROI.Method
The prospective study was approved by our Medical Ethics Committee. 104 patients with HCC confirmed by histopathological results were recruited. All patients underwent preoperative routine MR and IVIM sequence examination on a 3T MRI scanner (MAGNETOM Prisma; Siemens Healthcare, Erlangen, Germany), and IVIM used a research application multi-b-value DWI sequence with integrated-shimming. The parameters were: 8 b-values: 0 , 20 , 50 , 100 , 150 , 200 , 600 and 1000 s/mm2; TR: 4900 ms, TE: 57ms, FOV: 380 mm × 261 mm, matrix: 88×128, slice thickness: 5.0mm, bandwidth: 2442 Hz/pixel, acceleration factor: 2. The parameters derived from IVIM, D, D*, and f was fitting. A radiologist drew ROI manually to outline the tumor around the tumor margin on the original DW images (b = 1000 s/mm2) on whole tumor volume, avoiding the obvious hemorrhage, calcified, and necrotic areas. For all cases we used Otsu threshold algorithm to split tumor into low- and high-region on D, D*, and f, respectively. Finally, according to D (diffusion) and f (perfusion) maps, the whole tumor was segmented into four different subregions: D-Low/F-Low (LL), D-Low/f-Hight (LH), D-Hight/F-Low (HL) and D-Hight/f-Hight (HH) (Figure1,2). Then the mean value of the whole tumor and each region, volume and percentage of each region were estimated for the further analysis. The surgically resected hepatic specimens were used for the pathological evaluation. MVI was defined as a tumor within a vascular space lined by endothelium, and the MVI of tumor cells invasion into the portal branches and capillaries was pathologically examined by using the specimen samples. Student’s t test was used to compare the differences of parameters between MVI-negative and MVI-positive groups. The receiver operating characteristic (ROC) curves were generated based on the significant variables identified from the univariate analysis.Results
Of 104 patients, 49 cases (47.1%, mean age: 53.1±9.7 years) were diagnosed by histopathology as MVI-positive, and 55 cases (52.9%, mean age: 51.4±10.3 years) as MVI-negative. MVI-positive group had significant lower f_LH, Volumen_Percent_LH and significant higher Volumen_Percent_LL compared with those in MVI-negative group (P<0.05). There was no statistical significance in other parameters (P>0.05) (Table 1). f_LH had the best diagnostic performance for MVI (AUC:0.737,95%CI: 0.642~0.831,sensitivity:77.55%,specificity:63.64%,accuracy:70.19%), Volumen_Percent_LH and Volumen_Percent_LL also showed good diagnostic performance (AUC: 0.651, 95% CI: 0 .546~0.756; and AUC: 0.647, 95%CI: 0.541~0.754, respectively). The representative results are shown in Figure 3.Discussion
HCC becomes more poorly differentiated during hepatocarcinogenesis, the cellular density increase and and microvascular perfusion are also altered. In the most aggressive areas of the tumor, cell density is higher and angiogenesis is more vigorous, resulting in a decrease in D and an increase in f. On the contrary, D value increased in necrotic or well-differentiated areas, while f value decreased in hypovascular areas. According to the habitats analysis, four different subregions correspond to areas within the lesion with different combinations of tissue cellularity and microcirculation perfusion. Our data demonstrated that, in the D-Low/f-Hight(LH) region ,the perfusion parameters f in MVI-positive and MVI-negative showed statistical significance , which may be related with hemodynamic perfusion changes existing in the areas with dense tumor cells and abundant blood supply, the presence of tumor emboli or clusters of cancer cells in branches of hepatic vessels such as the portal vein, hepatic vein, and intracapsular vessel could restrict the perfusion3. In addition, in the area with high cell density, the distribution of microcirculation perfusion is inconsistent. In the MVI-positive group, the proportion of hyperperfusion (Volumen_Percent_LH) is lower and the proportion of hyperperfusion (Volumen_Percent_LL) is higher in this area, which seems to be related to the decrease of perfusion caused by microvascular embolism. However, the mean values of whole tumor of D, f and D* in MVI-positive and MVI-negative showed no statistical significance in our study, indicating that the average values can not reflect the biological characteristics and heterogeneity in the lesion.Conclusion
Our study found that Habitats Analysis using quantitative IVIM-derived D and f maps provide a more sophisticated biological information of tumor, which can be assessed as potential biomarkers for predicting MVI in HCC.Acknowledgements
No acknowledgement found.References
- Wei Y, Huang Z, Tang H, Deng L, Yuan Y, Li J, Wu D, Wei X, Song B. IVIM improves preoperative assessment of microvascular invasion in HCC. Eur Radiol. 2019 Oct; 29(10):5403-5414. doi: 10.1007/s00330-019-06088-w. Epub 2019 Mar 15. PMID: 30877465.
- Napel S, Mu W, Jardim-Perassi BV, Aerts HJWL, Gillies RJ. Quantitative imaging of cancer in the postgenomic era: Radio(geno)mics, deep learning, and habitats. Cancer. 2018 Dec 15; 124(24):4633-4649. doi: 10.1002/cncr.31630. Epub 2018 Nov 1. PMID: 30383900; PMCID: PMC6482447.
- Iima M, Le Bihan D. Clinical Intravoxel Incoherent Motion and Diffusion MR Imaging: Past, Present, and Future. Radiology. 2016 Jan;278(1):13-32. doi: 10.1148/radiol.2015150244. PMID: 26690990.
Figures
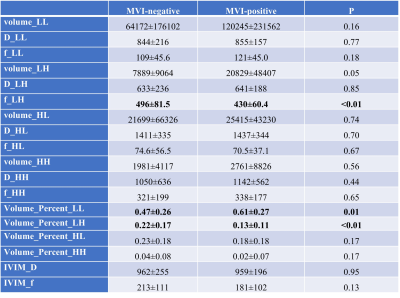
Table 1. Habitats analysis parameters of each region and mean value of the whole tumor between the MVI-negative and MVI-positive groups.
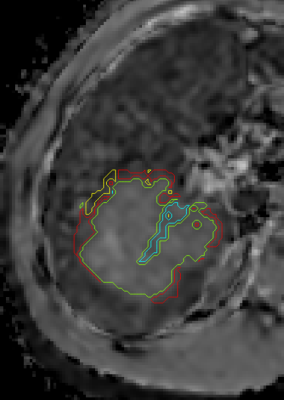
Fig 1. The whole tumor was segmented
into four different subregions used Otsu threshold
algorithm.
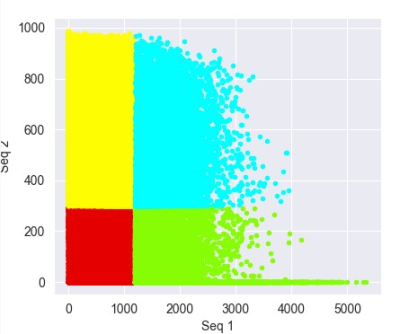
Fig 2. Red represents D-Low/F-Low (LL) habitat,yellow represents D-Low/f-Hight (LH) habitat, blue represents D-Hight/f-Hight (HH) habitat and green represents D-Hight/F-Low (HL) habitat.
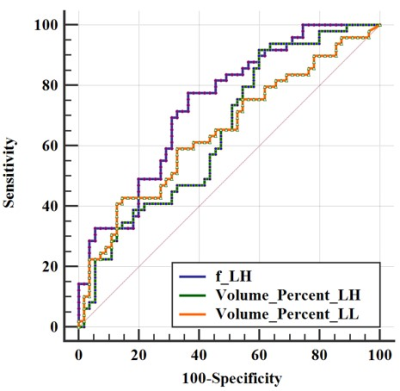
Fig 3. ROC curves of f_LH, Volumen_Percent_LH and Volumen_Percent_LL to distinguish MVI-positive and MVI-negative HCCs.
DOI: https://doi.org/10.58530/2023/3121