3051
Treatment response prediction of major depressive disorder using brain magnetic resonance imaging1Huaxi MR Research Center (HMRRC), Department of Radiology, West China Hospital of Sichuan University, Chengdu 610041, Sichuan, P.R. China, Chengdu, China
Synopsis
Keywords: Dementia, MR Value
We performed a meta-analysis by including published studies using machine learning for unrestricted modalities and interventions on magnetic resonance imaging (MRI) data to predict the effectiveness of treatment for patients with major depressive disorder (MDD). The results showed that the resting-state functional MRI (rs-fMRI) had higher predictive performance in the modality subgroups, suggesting brain rs-fMRI may have an advantage in prediction performance. Using machine-learning analysis to predict treatment effectiveness is promising, but should not yet be implemented into clinical practice.
Introduction
Despite the increasing availability of antidepressants and psychotherapy, MDD remains the leading cause of disability worldwide 1. Part of the reason for the continued onset of the disease is the difficulty of treatment selection. Patients may spend months to years searching for options before responding to treatment 2. Depression treatment could be improved by reducing unsuccessful treatment trials. A machine learning approach may lead to personalized treatment for patients by using brain MRI data to predict the effectiveness 3. Predicting treatment is helpful for selecting an effective treatment and shortening the course of disease. Therefore, we sought to quantify the accuracy of MRI data in effective prediction by using meta-analyses and to determine the limitations of existing methods.Methods
We included all published studies that used brain MRI data to predict the effectiveness of treatment for a meta-analysis. We conducted a systematic comprehensive literature search in PubMed, Embase, Web of Science, and Science Direct for studies through September 3, 2022, using keywords such as “depress*” or “major depress*” or “MDD” plus “treatment outcome” or “remission” or “remit*” or “response*” plus “magnetic resonance imaging” or “MRI” or “diffusion tensor imaging” or “DTI” or “neuroimaging”. The present study included all types of MRI modalities and interventions. We extracted information from the included studies for meta-analysis including sensitivity, specificity, and number of persons in response/remission or non-response/remission.We adopted the random effects of model of Reitsma to conduct bivariate analyses for sensitivity and specificity 4. We summarized the results as the logarithm of diagnostic odds ratios (DOR) and drew a forest map for univariate analysis. The accuracy of the meta-analysis was expressed by the sensitivity and specificity of the analysis using bivariate models, and the summary receiver operating characteristic curve (SROC) and area under the curve (AUC) 5.
To explore the impact of different MRI modalities and interventions, we conducted subgroup analyses based on intervention types (antidepressant; electroconvulsive therapy, [ECT]; cognitive behavioral therapy, [CBT]; repetitive transcranial magnetic stimulation, [r-TMS]) and modalities (structural MRI; rs-fMRI; task-based fMRI; and diffusion tensor imaging, [DTI]). We reported the I2 as a measure of heterogeneity. Furthermore, the Deeks’ funnel plot asymmetry test was performed to quantify publication bias 6.
Results
We included 39 studies that used different machine learning methods to predict the treatment effectiveness by using brain MRI data in 2579 participants with MDD. Among them, 17 studies (43.6%) used support vector machine model, 12 studies (30.8%) used logistic regression model, and 10 studies (25.6%) used other methods (random forest, decision tree, etc.).The meta-analytic results showed an AUC corresponding to SROC of 0.819, with sensitivity of 0.769 (95% CI [-0.042, 0.037]) and specificity of 0.739 (95% CI [-0.053, 0.047]) to predict the treatment effectiveness of MDD (Figure 1). The overall log (DOR) value of these 39 studies was 2.417 (95% CI [-0.327, 0.327]). Figure 2 showed the forest plot of the overall performances. The results of the heterogeneity test showed low heterogeneity (I2 = 7.293%) between studies. The Deeks’ test for funnel plot asymmetry showed asymmetry is not present in the effective sample size plot (P = 0.868), suggesting there’s no significant publication bias.
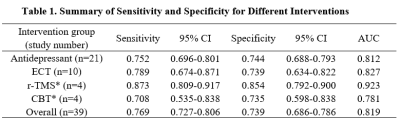
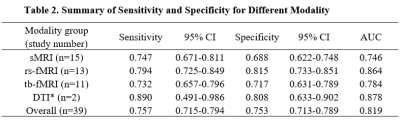
In the intervention subgroups, prediction performance of ECT (78.9% sensitivity,73.9% specificity, AUC 0.827) and antidepressant (75.2% sensitivity, 74.4% specificity, AUC 0.812) has higher performance, but there was no particular intervention showed higher predictive power than the others (Table 1). Among modality types, our results showed that rs-fMRI had higher predictive performance (79.4% sensitivity, 81.5% specificity, AUC 0.864) than other modalities (Table 2). For the CBT, r-TMS, and DTI subgroup analyses, the results shown in Tables 1 and 2 should be interpreted with caution, and further studies are needed because of the insufficient amount of study (n ≤ 4).
Discussion
The performance of predicting treatment effectiveness can achieve a high AUC, but we did not find a significant difference between two main interventions. This might be because patients with MDD tend to have drug treatment before ECT due to its side effect 7,8, leading to some overlap in treatment options for non-naive patients.For MRI modalities, the predictive performance of the rs-fMRI modality was higher than the others. The model of negative emotion processing is mainly a dynamic regulatory relationship between limbic and prefrontal regions 9,10, the dysfunction of which along with depressive symptoms is representative of MDD. Therefore, the included rs-fMRI studies analyzed the functional connectivity of these regions (hippocampus, amygdala, etc.) might be the reason for the higher performance for MDD treatment effectiveness.
The results of the study suggest that MRI has the potential in predicting treatment response but is not fully ready for guiding clinical decision-making. The sensitivity and specificity of prediction have not yet reached the critical value of clinical application proposed by the American Academy of Medicine in 2012 11. Further research in this field is needed to truly participate in clinical applications by using large sample data from multi-center.
Conclusion
The use of machine-learning analysis of brain MRI data to predict treatment response for MDD patients is promising but it needs more studies to get a replicated and validated result in favor of the implement of brain MRI into clinical practice.Acknowledgements
No acknowledgment was found.References
1. Roehrig C. Mental Disorders Top The List Of The Most Costly Conditions In The United States: $201 Billion. Health Aff (Millwood). 2016;35(6):1130-1135.
2. Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119-138.
3. Yahata N, Kasai K, Kawato M. Computational neuroscience approach to biomarkers and treatments for mental disorders. Psychiatry Clin Neurosci. 2017;71(4):215-237.
4. Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58(10):982-990.
5. Jones CM, Athanasiou T. Summary receiver operating characteristic curve analysis techniques in the evaluation of diagnostic tests. Ann Thorac Surg. 2005;79(1):16-20.
6. van Enst WA, Ochodo E, Scholten RJ, Hooft L, Leeflang MM. Investigation of publication bias in meta-analyses of diagnostic test accuracy: a meta-epidemiological study. BMC Med Res Methodol. 2014;14:70.
7. Steele JD, Farnan T, Semple DM, Bai S. Fronto-medial electrode placement for electroconvulsive treatment of depression. Front Neurosci. 2022;16:1029683.
8. Lin CH, Yang WC, Chen CC, Cai WR. Comparison of the efficacy of electroconvulsive therapy (ECT) plus agomelatine to ECT plus placebo in treatment-resistant depression. Acta Psychiatr Scand. 2020;142(2):121-131.
9. Underwood R, Tolmeijer E, Wibroe J, Peters E, Mason L. Networks underpinning emotion: A systematic review and synthesis of functional and effective connectivity. Neuroimage. 2021;243:118486.
10. Dimanova P, Borbás R, Schnider CB, Fehlbaum LV, Raschle NM. Prefrontal cortical thickness, emotion regulation strategy use and COVID-19 mental health. Soc Cogn Affect Neurosci. 2022;17(10):877-889.
11. First M, Botteron K, Carter C, et al. Consensus Report of the APA Work Group on Neuroimaging Markers of Psychiatric Disorders. APA Council on Research Consensus Paper. 2012.
Figures
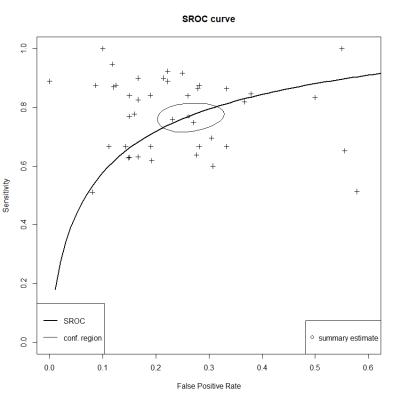
Figure 1. Overall Summary Receiver Operator Characteristic Curve. The area under the curve of overall performance is 0.819, Sensitivity is 0.769 (95% CI [-0.042, 0.037]), Specificity is 0.739 (95% CI [-0.053, 0.047]). The overall SROC curve is in black, and the confidence interval is the gray circle area. The horizontal axis represents the false positive rate (1-specificity), and the vertical axis for the sensitivity.
Abbreviations: Conf. region, the region of the confidence interval.
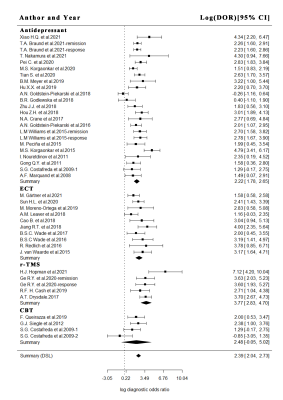
Figure 2. Overall Random Effect Model Forest Plot of logarithm of diagnostic odds ratios.
Abbreviations: CBT, cognitive behavioral therapy; DOR, diagnostic odds ratios; ECT, electroconvulsive therapy; r-TMS, repetitive transcranial magnetic stimulation.
*Note: indicates study samples insufficient with inaccurate or overfitting results.
Abbreviations: AUC, the area under the curve; CBT, cognitive behavioral therapy; CI, confidence interval; ECT, electroconvulsive therapy; r-TMS, repetitive transcranial magnetic stimulation.
*Note: indicates study samples insufficient with inaccurate or overfitting results.
Abbreviations: AUC, the area under the curve; CI, confidence interval; DTI, diffusion tensor imaging; rs-fMRI, resting-state functional magnetic resonance imaging; sMRI, structural magnetic resonance imaging; tb-fMRI, task-based functional magnetic resonance imaging.