3010
Combining CSF hydrodynamics and 4th ventricle outlet morphology improves predictive performance of decompression for CM-I patients1Department of Radiology, The Second Affiliated Hospital of Nanchang University, Nanchang, China, 2GE Healthcare, MR Research China, Beijing, China
Synopsis
Keywords: Neurofluids, Velocity & Flow
Foramen magnum decompression (FMD) is the most used surgical treatment for Chiari malformation type I patients. However, 25~33% of them have persistent symptoms after surgery. This study aimed at investigating the possibility to predict the FMD outcome by using cerebral fluid (CSF) hydrodynamics and 4th ventricle outlet morphology obtained from magnetic resonance imaging. 27 patients were included and 17 of them had improved outcomes after FMD. Our results showed the peak diastolic velocity of CSF in aqueduct and the width of 4th ventricle outlet were associated with the FMD outcome and combining them can improve the prediction performance.Introduction
It is generally known that foramen magnum decompression (FMD) is the most recognized and commonly used surgical treatment for patients with Chiari malformation type I (CM-I)1. However, symptom recurrence or persistence occurs in some patients after surgery, which varies between 25% and 33% in previous reports2, indicating that surgical was not the optimum choice for every patient. Hence, available, and accurate preoperative identification methods to determine which patients would benefit from FMD are indispensable.Previous study using magnetic resonance imaging (MRI) shows some morphologic features of the brain and cervical vertebrae are associated with surgical treatment prognosis of CM-I3,4. The narrow of 4th ventricular outlet is the characteristic of CM-I5 . The crowded posterior fossa of CM-I patients was confirmed to lead to aberrant CSF flow dynamics6,7. However, few studies have evaluated the role of CSF hydrodynamics and 4th ventricle outlet morphology in predicting the outcome of FMD treatment. In this study, structural and phase contrast cine (PC-cine) MRI were used to extract the morphology and flow dynamic features, respectively. The features which could be used as predictor of the FMD outcome were investigated.
Material and Methods
Patients27 CM-I patients (median age, 47 years; interquartile range, 39–50.5 years; 12 men and 15 women) and 23 volunteers (median age, 29 years; interquartile range, 26–52.5 years; 8 men and 15 women) were included. All patients received telephone follow-ups in April 2022. The phone interview was performed by an author using the CCOS. The patients were grouped into improved outcome (CCOS≥13) and poor outcome (CCOS<13) groups.
MRI experiment
Images were acquired on a 3.0T MR scanner (Discovery 750w; GE Healthcare, Waukesha, USA) with a 24-channel head and neck unit coil. The PC-cine MRI including 3D Fiesta and 3D-Cube was acquired in the midportion of the aqueduct and the fourth ventricle outlet. In addition, a series of conventional MRI sequences, including axial T1WI, T2WI, or FLAIR, were scanned, and a sagittal scan of the cervical vertebrae or spine MRI was performed in the CM-I.
Data analysis
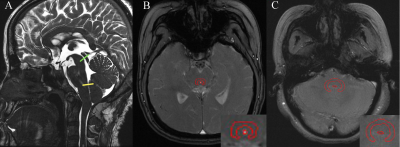
All PC-cine MRI data were transferred to GE AW 4.4, The region of interest (ROI) was manually defined on magnitude images (Figure 1) by two neuroradiologists who were blinded to the treatment outcomes. The CSF parameters available were the peak systolic velocity (PSV), the peak diastolic velocity (PDV), the average velocity (AV), the net flow (NF), the peak systolic flow (PSF) and the peak diastolic flow (PDF). Anatomical measurements were performed by the above two radiologists, and the average values of the two measurements were used for statistical analysis.
Statistical analysis
Using SPSS software (version 26.0) and R software, Mann-Whitney U tests were used for continuous variables, and the χ2 or Fisher exact test were used for categorical variables between the groups of healthy controls and CM-I patients and between the improved and poor prognoses subgroups. Logistic regression analysis was performed to determine the independent preoperative predictors for FMD prognosis in CM-I. The predictive performance was evaluated with ROC, calibration and decision curves. The intraclass correlation coefficient (ICC) was used to evaluate the consistency between two observers.
Results
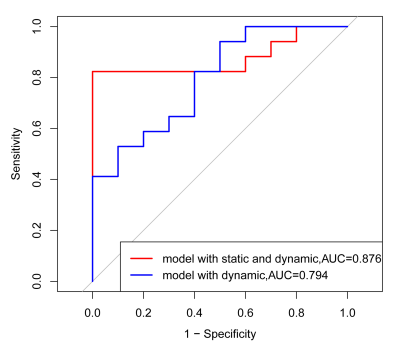
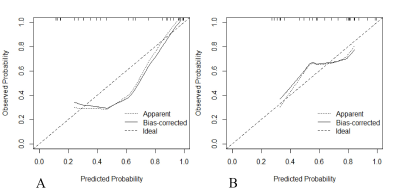
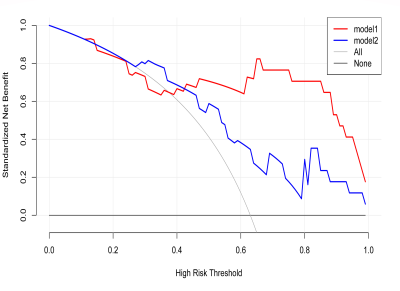
Of the 27 patients, 63% (17/27) had improved outcomes, and 37% (10/27) had poor outcomes. The peak diastolic velocity (PDV) of the aqueduct midportion (OR, 5.17; 95% CI: 1.08, 24.70; P=0.039) and the fourth ventricle outlet diameter (OR, 7.17; 95% CI: 1.07, 48.16; P=0.043) were predictors of FMD outcome. For the model based on CSF dynamic parameters, only the PDV of the middle portion of the aqueduct (OR, 4.54; 95% CI: 1.11, 18.58; P=0.035) was an independent risk factor. The predictive model based on dynamic and morphological features yielded an AUC of 0.876 (95% CI:0.74,1.00) and accuracy of 88.89% (95% CI:0.71,0.98) which were better than that of the model based on CSF dynamic parameters only, with AUC of 0.794 (95% CI: 0.62, 0.97) and accuracy of 77.78% (95% CI:0.58,0.91) (Figure 2). The AUC showed no significant differences between the two models (P =0.36).Compared with the model based on CSF hydrodynamic, the model combining CSF hydrodynamic and morphological characteristics yielded a continuous net reclassification index (NRI) of 1.01 (95% CI: 0.35, 1.67, P=0.003) and integrated discrimination improvement (IDI) of 0.214 (95% CI: 0.07, 0.35, P =0.003). The calibration curve indicating that there was no significant difference between the combining model and the ideal perfect model (Figure 3). The decision curve revealed that the net benefit of the combine model was higher than that of the extreme curves and the single dynamic model in a range of 0.5 to 1.0 risk thresholds (Figure 4).
Discussion and Conclusions
In this study, we investigate the role of the 4th ventricle outlet morphology and CSF hydrodynamics measured by MRI in predicting the FMD outcome of CM-I patients. Our results demonstrated that larger fourth ventricle outlet anteroposterior diameter and higher PDV of the aqueduct midportion were associated with improved outcomes. The combination of the two features improved the prediction performance of FMD surgical treatment. Our research helps provide new preoperative evaluation for patients' surgical selection, formulate personalized treatment plans, and obtain more significant curative effects on disease. Further work is warranted to collect more cases and conduct prospective internal and external verification.Acknowledgements
No acknowledgement found.References
1. Bartoli A, Soleman J, Berger A, et al. Treatment Options for Hydrocephalus Following Foramen Magnum Decompression for Chiari I Malformation: A Multicenter Study. Neurosurgery. Apr 1 2020;86(4):500-508. doi:10.1093/neuros/nyz211
2. Dyson EW, Chari A, Toma AK, Thorne LW, Watkins LD. Failed Foramen Magnum Decompression in Chiari I Malformation Is Associated With Failure to Restore Normal Intracranial Compliance: An Observational Cohort Study. Neurosurgery. Jun 1 2020;86(6):E552-E557. doi:10.1093/neuros/nyaa079
3. Abdallah A, Cinar I, Gundag Papaker M, Guler Abdallah B, Sofuoglu OE, Emel E. The factors affecting the outcomes of conservative and surgical treatment of chiari i adult patients: a comparative retrospective study. Neurol Res. Feb 2022;44(2):165-176. doi:10.1080/01616412.2021.1967681
4. Alford EN, Atchley TJ, Leon TJ, et al. Imaging characteristics associated with surgery in Chiari malformation type I. Journal of neurosurgery Pediatrics. Apr 23 2021;27(6):620-628. doi:10.3171/2020.9.Peds20347
5. Seaman SC, Li L, Menezes AH, Dlouhy BJ. Fourth ventricle roof angle as a measure of fourth ventricle bowing and a radiographic predictor of brainstem dysfunction in Chiari malformation type I. Journal of Neurosurgery: Pediatrics. 2021;28(3):260-267. doi:10.3171/2021.1.Peds20756
6. McGirt MJ, Atiba A, Attenello FJ, et al. Correlation of hindbrain CSF flow and outcome after surgical decompression for Chiari I malformation. Childs Nerv Syst. Jul 2008;24(7):833-40. doi:10.1007/s00381-007-0569-1
7. Quigley MF, Iskandar B, Quigley ME, Nicosia M, Haughton V. Cerebrospinal fluid flow in foramen magnum: temporal and spatial patterns at MR imaging in volunteers and in patients with Chiari I malformation. Radiology. Jul 2004;232(1):229-36. doi:10.1148/radiol.2321030666
Figures