2965
Feasibility study of predicting invasive placenta accreta and adverse clinical outcomes based on quantitative MRI parameters1Department of Radiology, Renmin Hospital of Wuhan University, Wuhan, China, 2MR Research, GE Healthcare, Beijing, China
Synopsis
Keywords: Placenta, Placenta
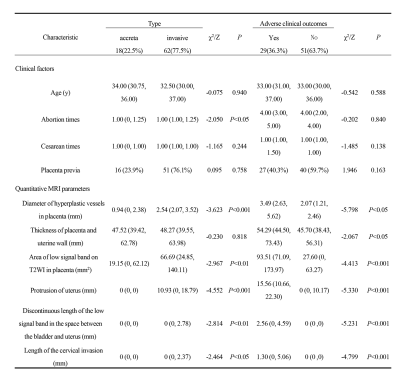
Clear prenatal diagnosis and correct intraoperative treatment can ensure the safety of the fetus and pregnant women. Logistic regression analysis based on quantitative MRI parameters showed that abortion times, diameter of hyperplastic vessels in placenta and protrusion of uterus were independent risk factors for invasive placenta accreta. Diameter of hyperplastic vessels in placenta, area of low signal band on T2WI in placenta and protrusion of uterus were independent risk factors for predicting adverse clinical outcomes. Our study showed the accuracy of the binary Logistic regression model in prediction of placenta type and adverse clinical outcome was 91.3%.Introduction and Purpose
Invasive placenta accreta is one of the main causes of obstetric massive bleeding, hysterectomy and even maternal death [1, 2]. Clear prenatal diagnosis and correct intraoperative treatment are the key to reduce postpartum massive bleeding, hysterectomy and postoperative adverse events of women with placenta accreta, and can ensure the safety of the fetus and pregnant women. At present, there has been no report of quantitative MRI parameters to predict invasive placenta accreta and adverse clinical outcomes. This study attempted to construct a risk prediction model based on quantitative MRI parameters to predict adverse clinical outcomes of placenta accreta, and also evaluate the prediction performance of the model on clinical risk factors.Method
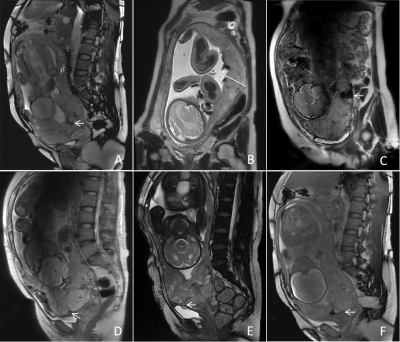
The clinical and MRI data of 80 patients in our hospital were retrospectively included in this study. The MRI image features of each patient were recorded, including the diameter of blood vessels with placental dysplasia, the thickness of placental and uterine wall, the area of low signal zone in placental T2WI, the degree of external protrusion of uterus, the discontinuous length of low signal zone in the space between bladder and uterus, and the length of cervical invasion (Figure 1). Binary logistic regression analysis was used to examine the performance of MRI image features in predicting the types of placenta accreta and independent risk factors for adverse clinical outcomes, and then a differential model was constructed. The area under the curve (AUC), sensitivity, specificity and Youden index were evaluated for the diagnostic performance of receiver operating characteristic (ROC) curve model. The stability of the regression model was internally verified by Bootstrap.Results
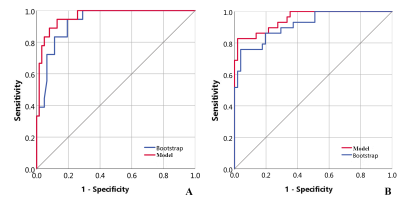
The median age of the 80 patients was 33 years old (20-44 years old), and the median gestational age was 36.1 weeks (28.0 - 39.4 weeks). There were 18 cases of accreta (22.5%) and 62 cases of invasive placenta accreta (77.5%). Binary Logistic regression analysis showed that abortion times [OR (95%CI): 4.271(1.226-14.876)], diameter of hyperplastic vessels in placenta [OR (95%CI): 3.789(1.367-10.501)], protrusion of uterus [OR (95%CI): 1.432(1.088-1.885)] were independent risk factors for invasive placenta accreta, all P <0.05. Diameter of hyperplastic vessels in placenta [OR (95%CI): 0.053(0.009-0.314)], area of low signal band on T2WI in placenta [OR (95%CI): 1.016(1.004-1.029)], and protrusion of uterus [OR (95%CI): 0.839(0.727-0.968)] were independent risk factors for predicting adverse clinical outcomes (all P <0.05). The accuracy of the model to predict types of placenta and occurrence of adverse clinical outcomes was 91.3% and this model was stable by Bootstrap analysis (Figure 2).Discussion
At present, selection of MRI features, qualitative and quantitative parameters for the MRI scoring system and regression model in the classification of placenta accrete and adverse clinical outcomes did not come to an agreement. Normal placenta also shows vascular signs, local placental thickening, myometrium thinning and physiological heterogeneity on MRI [6], so these signs cannot be used to determine the status of placenta. However, most previous studies have combined a variety of qualitative MRI features to establish models [3-5]. The weight of each MRI sign to predict placenta accreta and clinical outcome was different, and equal weight of each sign led to bias in the scoring model. Therefore, the diagnostic value of MRI signs largely depends on the observer’s experience [7]. In contrast, the reproducibility and stability of quantitative MRI parameters that are not affected by observer experience are higher. In this study, the binary logistic regression analysis based on quantitative MRI parameters for invasive placenta accreta and adverse clinical outcomes showed relatively objective with high sensitivity (94.4%, 98.0%) and specificity (85.5%, 82.8%) . When the value obtained in our model was greater than the predicted critical value, there is a high possibility of invasive placenta accreta and adverse clinical outcomes, suggesting that it is necessary to fully prepare the blood transfusion or hysterectomy materials before obstetrics.Conclusion
The binary logistic regression model based on quantitative MRI parameters showed a good performance on predicting invasive placenta accreta and adverse clinical outcomes, and could improve the overall diagnostic efficiency.Acknowledgements
I would like to thank my supervisor Professor Yunfei Zha for his guidance and Weiyin Vivian Liu from GE Healthcare for her technical assistance.References
[1] D'Arpe S, Franceschetti S, Corosu R, et al. Emergency peripartum hysterectomy in a tertiary teaching hospital: a 14- year review[J] .Archb Gynecol Obstet, 2015, 291(4):841-847.
[2] Jauniaux E, Bhide A, Kennedy A, et al. FIGO consensus guidelines on placenta accreta spectrum disorders: Prenatal diagnosis and screening[J]. Int J Gynaecol Obstet, 2018, 140(3):274-280.
[3] Ueno Y, Maeda T, Tanaka U, et al. Evaluation of interobserver variability and diagnostic performance of developed MRI based radiological scoring system for invasive placenta previa[J]. J Magn Reson Imaging, 2016, 44(3):573-583.
[4] Lim G, Horowitz JM, Berggruen S, et al. Correlation of probability scores of placenta accreta on magnetic resonance imaging with hemorrhagic morbidity[J]. J Clin Anesth, 2016, 34:261-269.
[5] Delli Pizzi A, Tavoletta A, Narciso R, et al. Prenatal planning of placenta previa: diagnostic accuracy of a novel MRI-based prediction model for placenta accreta spectrum (PAS) and clinical outcome[J]. Abdom Radiol (NY), 2019, 44(5):1873-1882.
[6] D’Antonio F, Iacovella C, Palacios-Jaraquemada J, Bruno CH, Manzoli L, Bhide A. Prenatal identification of invasive placentation using magnetic resonance imaging: systematic review and meta-analysis[J]. Ultrasound Obstet Gynecol, 2014, 44(1):8-16.
[7] Alamo L, Anaye A, Rey J, et al. Detection of suspected placental invasion by MRI:do the results depend on observer’ experience[J]? Eur J Radiol, 2013, 82(2):e51-57.
Figures