2880
Three Delineating Radiomics Models Based on MR-determined Metastatic Lymph Nodes for Prognostic Prediction in Nasopharyngeal Carcinoma1Sun Yat-sen University Cancer Center, Guangzhou, China, 2Philips Healthcare, Guangzhou, China, 3Hainan General Hospital (Hainan Affiliated Hospital of Hainan Medical University), Haikou, China
Synopsis
Keywords: Radiomics, Cancer, Nasopharyngeal Carcinoma
The purpose of this study was to assess the performance of radiomic models based on MR-determined metastatic lymph nodes phenotype in predicting the prognosis of nasopharyngeal carcinoma (NPC) with three different feature selection methods: all lymph nodes (ALN), the largest lymph node (LLN), and the largest slice of the largest lymph node (LSLN). The results showed that LSLN radiomic features showed better accuracy in predicting the overall survival (OS).Objectives
Nasopharyngeal carcinoma (NPC) is characterized by a high probability of early lymphatic spread and distant metastasis1,2, with more than 70% of patients initially diagnosed with locally advanced disease. Despite the continuously increasing knowledge of tumor biology3, the evolution of comprehensive treatment, and the popularity of magnetic resonance (MR) examination, the prognosis of patients with NPC is still poor4,5. Accurate prediction of the prognosis of nasopharyngeal carcinoma (NPC) is important for treatment planning. Magnetic resonance (MR) based radiomics models of metastatic lymph nodes hold the potential for personalized prediction, but the performance of the lymph-node-based models, and the effect of different delineation methods on the models’ performance, remain unknown. The aim of this study was to evaluate the performance of radiomics models based on MR-determined metastatic lymph nodes phenotype in predicting the prognosis of NPC with three different feature selection methods: all lymph nodes, the largest lymph node, and the largest slice of the largest lymph node.Materials and Methods
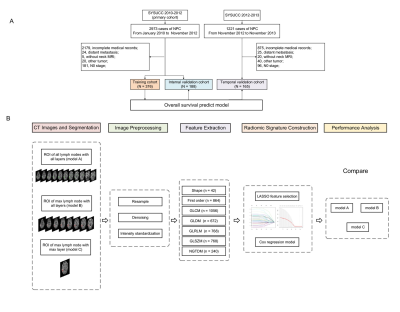
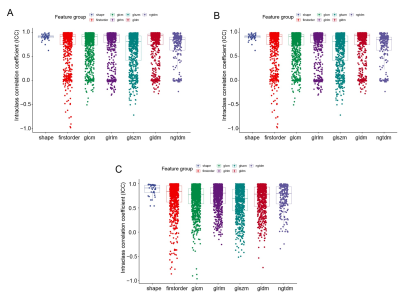
This retrospective study included T1-weighted imaging, T2-weighted imaging, and contrast-enhanced T1-weighted imaging of consecutive, newly diagnosed, non-metastatic NPC. Radiomics features were extracted from all lymph nodes, the largest lymph node, and the largest slice of the largest lymph node, annotated by a fellowship-trained radiologist. The radiomics signatures of all lymph nodes, the largest lymph node, the largest slice of the largest lymph node, the clinical model, and the merged models, combining radiomics signatures and clinical factors, were developed in the training cohort for predicting overall survival (OS). The least absolute shrinkage and selection operator (LASSO) method was applied for feature selections and modeling, and Harrell’s concordance index (C-index) was used to evaluate the model’s discrimination. The accuracy of the models for prediction was verified in internal and temporal validation cohorts.Results
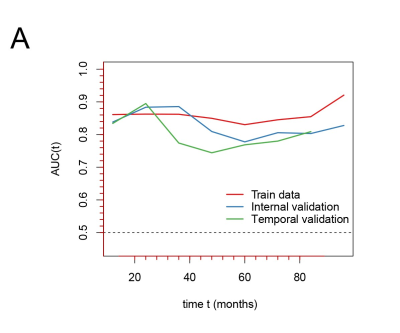
Between January 2010 and November 2012, the data of 376 and 188 patients were retrospectively analyzed in the training and internal validation cohorts, respectively. The data of 165 eligible patients, seen after November 2012, were analyzed as a temporal validation cohort. The largest slice of the largest lymph node radiomics signature demonstrated better accuracy for the prediction of OS compared to the radiomics signatures of all lymph nodes and the largest lymph node in the training cohort (0.761 vs. 0.739 vs. 0.704), in the internal validation cohort (0.732 vs. 0.640 vs. 0.669), and in the temporal validation cohort (0.703 vs. 0.606 vs. 0.656), no significant difference of differences between the largest lymph node and the largest slice of the largest lymph node signatures (all P >.05). The radiomics nomogram combining the largest slice of the largest lymph node radiomics signature and clinical factors demonstrated significantly better performance than the clinical model (all P <.05).Conclusions
A radiomics model, constructed with the largest slice of the largest lymph node features, demonstrated comparable performances with those constructed with features from all lymph nodes and the largest lymph node. The nomogram with the largest slice of the largest lymph node signature and clinical factors was able to predict OS with high accuracy and robustness and could therefore provide a time-saving and efficient tool to assist with personalized prediction of NPC.Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.References
1. Huang L, Zhang Y, Liu Y, et al. Prognostic value of retropharyngeal lymph node metastasis laterality in nasopharyngeal carcinoma and a proposed modification to the UICC/AJCC N staging system. Radiother Oncol. 2019;140:90-7.
2. Chen YP, Chan ATC, Le QT, et al. Nasopharyngeal carcinoma. Lancet. 2019;394(10192):64-80.
3. Lee CK, Jeong SH, Jang C, et al. Tumor metastasis to lymph nodes requires YAP-dependent metabolic adaptation. Science. 2019;363(6427):644-9.
4. Lai SZ, Li WF, Chen L, et al. How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients? Int J Radiat Oncol Biol Phys. 2011;80(3):661-8.
5.Lee N, Harris J, Garden AS, et al. Intensity-modulated radiation therapy with or without chemotherapy for nasopharyngeal carcinoma: radiation therapy oncology group phase II trial 0225. J Clin Oncol. 2009;27(22):3684-90.
Figures