2873
Physiological variability of the tympanic membrane temperature as an RF safety metric assessment
Caroline Le Ster1, Mikhail Kozlov2, Alexandre Vignaud1, and Nicolas Boulant1
1University of Paris‐Saclay, CEA, CNRS, BAOBAB, NeuroSpin, Gif-sur-Yvette, France, 2Department of Neurophysics, Max Plank Institut for Human Cognitive and Brain Sciences, Leipzig, Germany
1University of Paris‐Saclay, CEA, CNRS, BAOBAB, NeuroSpin, Gif-sur-Yvette, France, 2Department of Neurophysics, Max Plank Institut for Human Cognitive and Brain Sciences, Leipzig, Germany
Synopsis
Keywords: Safety, Thermometry
RF exposure during MR exams induces heating of the exposed tissues. Measurement of tympanic membrane temperature with an infrared sensor has been used to estimate non-invasively the global RF-induced temperature rise. In this study, the tympanic membrane temperature was measured before and after having the volunteers lying for 15 minutes with earplugs with neither an RF nor a static magnetic field. Large physiological variations of temperature rise were observed across the volunteers after this dummy “exposure”, showing the low reliability of this metric to measure small temperature rises, that make it problematic for RF-induced temperature rise estimation.Introduction
Tympanic membrane temperature has been used to measure the small temperature rise induced by RF-power deposition during MR exams in previous studies [1-3]. The tympanic membrane is irrigated by the carotid artery, and as such its temperature may reflect the one of the brain. However, tympanic membrane temperature has been shown to vary with other parameters such as scalp and room temperatures [4]. The aim of the current study was thus to measure the physiological variability of the tympanic membrane temperature with volunteers merely lying with earplugs in a mock scanner in order to assess the reliability of this metric for RF safety evaluation.Methods
Experiments were performed on 15 volunteers (7 women/8 men). The tympanic membrane temperature was measured in their right and left ears before (= initial temperature) and after (= final temperature) experiment using an infrared thermometer (Riester GmbH, Jungingen, Germany) having a precision of 0.2°C. The experiment consisted in having the volunteers lying in a ‘0T’ mock scanner (used for children habituation, see Figure 1) during 15 minutes with earplugs to assess the reliability of this method to evaluate temperature rises induced by RF fields. In 5 volunteers, measurements were repeated a second time on a different day to assess reproducibility. No room temperature acclimation was performed before the measurements and the volunteers were instructed not to sleep during the experiment. The volunteers were not covered with a blanket. Initial and final temperatures measured in the right and left ears of the volunteers were compared using paired t-tests with bilateral distribution, the significance threshold was set to 5%.Results
Tympanic membrane initial temperatures showed large physiological variations across volunteers, with values ranging from 35.5°C to 37.1°C. There was no significant variation between the first and the second measurement for subjects in which tympanic temperature measurement was performed twice (p-value = 0.3). When averaged over the subjects, the tympanic membrane temperature revealed no significant difference between the right ear and the left ear for the initial (Ti,right = 36.4±0.6°C vs. Ti,left = 36.2±0.6°C, p=0.6) and final (Tf,right = 36.4±0.6°C vs. Tf,left = 36.3±0.6°C, p=0.3) measurements (Figure 2a). The difference between the initial and final tympanic membrane temperature measured before and after lying could reach -1.3°C to +0.6°C in some subjects, thereby demonstrating relatively large intersubject physiological variability (Figure 2b). Relevant positive temperature changes therefore did occur although no RF fields were applied. When averaged over the population, the temperature variation was statistically not significant (Figure 2a, p=0.7). The large variability however would make group analysis problematic to detect with large confidence sub-degree temperature rises as expected in MR exams.Conclusion
A large variability of tympanic membrane temperature rise was observed in the current study merely after lying 15 minutes with earplugs in a “mock” scanner. The reported intra- and inter-subject variations occurred most likely due to physiological variations. While no systematic temperature rise could be measured on average over the population, the large physiological intersubject variations reported here before and after “exposure” make quantitative analysis problematic when this metric is used to assess small temperature rises induced by RF fields in MRI. As such, caution is advised regarding the data interpretation unless the proper statistical analysis is performed.Acknowledgements
This work received financial support from the European Union Horizon 2020 Research and Innovation program under grant agreement no. 885876 (AROMA).References
1. Shellock, F. G., Schaefer, D. J., & Kanal, E. (1994). Physiologic responses to an MR imaging procedure performed at a specific absorption rate of 6.0 W/kg. Radiology, 192(3), 865-868.
2. Shrivastava, D. (2020). On the Choice of RF Safety Metric in MRI: Temperature, SAR, or Thermal Dose. Safety and Biological Effects in MRI, 173.
3. van den Brink, J. S. (2019). Thermal effects associated with RF exposures in diagnostic MRI: overview of existing and emerging concepts of protection. Concepts in magnetic resonance part b, 2019.
4. Wissler E.H. (2018) Temperature Measurement. In: Human Temperature Control (pp. 41-76). Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-57397-6_3.
Figures

Figure 1: The experimental setup consisted in a mock MR scanner used for children habituation, where the volunteers could lie as if in a standard MR scanner, with earplugs.
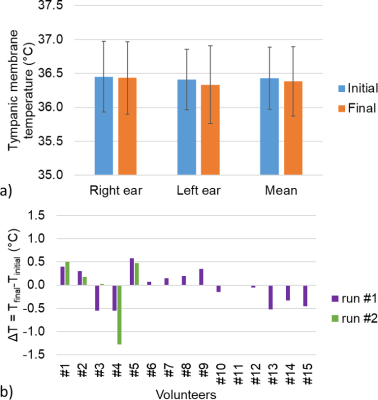
Figure 2: a) Barplot of the averaged tympanic membrane temperature measured over 15 volunteers in their right and left ears, and averaged over the ears, before and after lying 15 minutes with earplugs. b) Individual variations averaged over the right and left ears. While no systematic effect could be detected on average over the population, large physiological changes occurred on some subjects including sometimes positive changes, although no RF field was applied. A repeatability measurement was performed in 5 subjects.
DOI: https://doi.org/10.58530/2023/2873