2799
Radiation Dependent Demyelination in Normal Appearing White Matter in Glioma Patients, Determined Using Quantitative MRI1Department of Medical Radiation Physics, and Department of Health, Medicine and Caring Sciences, Linköping University, Linköping, Sweden, 2Center for Medical Image science and Visualization (CMIV), Linköping University, Linköping, Sweden, 3Department of Radiology in Linköping, and Department of Health, Medicine and Caring Sciences, Linköping University, Linköping, Sweden
Synopsis
Keywords: White Matter, Radiotherapy
Adding quantitative MRI to existing examinations for patients with malignant glioma is valuable for observing changes in tissue specific parameters such as R1, R2, proton density and myelin concentration. Changes observed in this study, with a decrease of myelin concentration and increase of proton density, in normal appearing white matter can be interpreted as a demyelination caused by radiation therapy. For low doses (<30 Gy), but not for high (>30 Gy) the myelin concentration returns to baseline.Background
Despite an aggressive treatment, about 50% of patients diagnosed with glioma decease within 5 years. Therefore, improving both diagnostic imaging and treatments are essential for these patients. It is not only a prolonged survival that is desirable, but also a good quality of life. In many cases, patients undergo surgery, subsequently followed by a combination of chemotherapy and radiation therapy. The ionising radiation is focused on the pre-surgical location of the tumour, including margins into unaffected areas. The treatment is delivered five times a week during six weeks, each day a dose of 2 Gy is given up to a total of 60 Gy. A disadvantage of the interventions is that the therapy affects not only the tumour, but also to some extent the surrounding tissue. Which can result in cognitive dysfunction thus effecting quality of life. Standard clinical routine prescribes conventional MRI in the pre- and post-operative setting and also during follow-up after treatment. In this study relaxometry was used to analyse normal appearing white matter (NAWM) after radiation therapy in gliomas.Aim
Detecting changes, such as demyelination, in normal appearing white matter (NAWM) caused by radiation therapy using quantitative MRI (qMRI).Material & methods
The qMRI sequence SyMRI MaGiC (GE Healthcare) was added to the conventional clinical MR-protocol when scanning 10 high grade glioma patients. The axial scans had a FOV of 220 x 180 mm2 and voxel size of 0.43 x 0.43 x 5 mm3. A total of 24 slices were collected with a total scan time of 5:55 min. Images reconstructed/calculated were T1- and T2- maps, proton density map and myelin concentration map, as well as synthetic T2-weighted images. Images were reconstructed using SyMRI (SyntheticMR AB). Relaxation rates R1 and R2 were calculated from the reconstructed T1 and T2-maps. Changes in NAWM were detected by comparing differences of mean values in ROIs from different time-points, compared with the pre-operative MRI. ROIs were placed in up to 14 anatomical regions. ROIs were not placed if tumour or oedema was/had been present at that location. An example of the T2-weighted images with ROI-placement and absorbed dose as an overlay is shown in Fig. 1. The quantitative maps of R1, R2, proton density and myelin concentration are also shown for one patient with four follow-up examinations. Association between changes were then analysed as a function of absorbed dose from radiation therapy and time after treatment.Results
A significant decrease in myelin concentration (-2.2%) between pre-operative and 1st follow-up images was observed, and also a corresponding increase in PD (1.5%). No significant changes in R1 were observed although there was a significant change (0.3 s-1) in R2. Associations between dose and time are shown in Fig 2. With time and low dose, the PD-value and myelin concentration returned to baseline, while for high doses (>30 Gy) there was an increase with time. R2 returned to baseline with time, but independent of dose level. A more pronounced change was seen for higher doses.Discussion and conclusion
qMRI can be used succesfully in a clinical setting during longitudinal follow-up after therapy of glioma patients for detecting changes in tissue parameters such as R2, PD and myelin concentration. It is important to note that the observed changes was a consequence of chemoradiotherapy; they were not observed in the post-operative images after surgery. After therapy a demyelination was observed and for low doses, but not for high doses, myelin concentration returned to baseline with time. The severity of the demyelination and remyelination depended on the accumulated amount of ionising radiation. Our analysis showed that the effects were not due to oedema, as R2 did not decrease.Acknowledgements
The study was approved by the regional ethics board, ID: 2011/406-31 (IB).
This work was conducted with support from ALF Grants, Region Östergötland, and Swedish Childhood Cancer Fund (‘Barncancerfonden’).
References
Warntjes, J.B., O. Dahlqvist, and P. Lundberg, Novel method for rapid, simultaneous T1, T2*, and proton density quantification. Magn Reson Med, 2007. 57(3): p. 528-37.
Warntjes, J.B., et al., Rapid magnetic resonance quantification on the brain: Optimization for clinical usage, in MAGNETIC RESONANCE IN MEDICINE. 2008, John Wiley & Sons, Ltd: United States. p. 320-329.
Figures
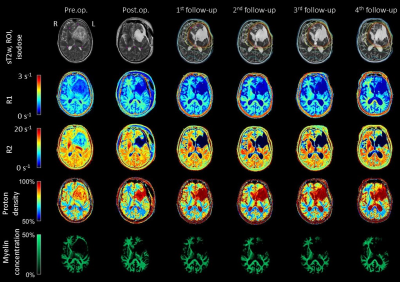
Fig. 1. MR-images at different time-points; pre-operative, post-operative, 1st follow-up, 2nd follow-up, 3rd follow-up and 4th follow-up. Top row shows synthetic T2-weighted images (sT2w), small circular pink ROIs in white matter, and isodose levels from radiation therapy corresponding to 10, 20, 30, 40, 50 and 57 Gy. ROI may not be in the same slice in all occasions due to reconstruction angle and suppression of surrounding tissue due to tumour. Second to fifth row are MRI images corresponding to R1-map, R2-map, proton density map and myelin concentration maps.
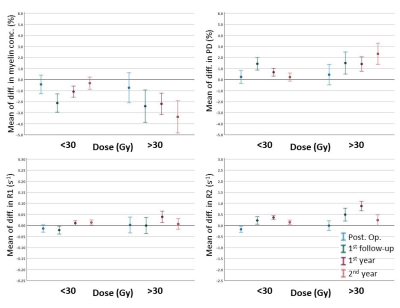
Fig. 2. Changes in myelin concentration (upper left), proton density (PD) (upper right), R1 (lower left) and R2 (lower right). The changes corresponded to the mean of differences in the ROIs between different time points and pre-operative image. The differences are shown for ROIs receiving less or more than 30 Gy. The interval shown is the 95% confidence interval for the mean.