2733
MR-derived breast density (MagDensity) enables reliable density measures across field strengths and vendors1Biomedical Engineering, Stony Brook University, Stony Brook, NY, United States, 2Radiation Oncology, Stony Brook Medicine, Stony Brook, NY, United States, 3Radiology, Stony Brook Medicine, Stony Brook, NY, United States
Synopsis
Keywords: Breast, Breast
The current standard of care for breast density assessment using mammography according to the Breast Imaging Reporting and Data System (BI-RADS) is subjective and can also suffer from intra- and inter-reader variability. Quantitative measurement of breast density is crucial for personalized risk assessment and longitudinal monitoring. Our team has previously developed a quantitative, MR-derived BD (MagDensity) measurement based on fat-water decomposition, which has shown high accuracy and test-retest reproducibility within a single scanner. In order for this measure to be practical for clinical adoption, this study aims to determine the reliability of MagDensity across scanners, field strengths, and vendors.Introduction
Quantitative measurement of breast density (BD) is crucial for personalized risk assessment and longitudinal monitoring. A reliable and accurate BD measure is desired in clinical practice. For instance, changes in BD have been examined in clinical trials as surrogate measures for evaluating the efficacy of hormone therapies (e.g., tamoxifen and aromatase inhibitors) used for the prevention and treatment of breast cancer1, 2. Our team has previously developed a quantitative MR-derived BD (MagDensity) measurement3 based on fat-water decomposition. The test-retest reliability of MagDensity has shown to be high on the same scanner; however, this presents a logistic challenge in clinical practice or research studies to always schedule patients on the same scanner each time. Therefore, the aim of this study is to determine the reliability of MagDensity across scanners, field strengths, and vendors for clinical/research adoption.Methods
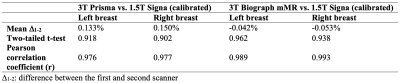
Ten healthy volunteers were recruited, and each underwent three 5-minute fat-water breast MRI scans on three different scanners from two major vendors (3T Siemens Prisma, 3T Siemens Biograph mMR, and 1.5T GE Signa). Acquisition parameters are summarized in Table 1. Data for each participant were acquired within 3 hours to avoid changes in BD (e.g., menstrual cycle, weight changes). Fat-water separation was performed as described in ref.4 to generate fat-only and water-only images. MagDensity was calculated for data obtained from the three scanners. The details of the calculation were described in ref.3. Agreement between measures was assessed using the mean difference, two-tailed t-test, and Pearson’s correlation. The significance level was set at 0.05.Results
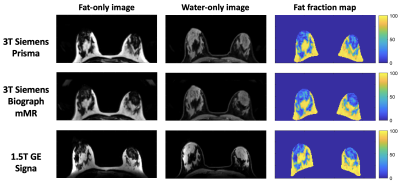
Figure 1 shows the reconstructed fat-only and water-only images, as well as the fat fraction maps (representing the relative percentage amount of fat signal in each voxel) used for MagDensity calculation.For MagDensity measures between the same field strength (3T) and the same vendor (Siemens), the observed cross-scanner mean differences were small (< 0.5%), this is similar to the test-retest variability of the same scanner previously reported in ref.5. Pairwise t-test showed no statistically significant difference between the MagDensity measures of 3T Siemens Prisma and 3T Siemens Biograph mMR (P > 0.05; r > 0.99) (Figure 2). The results are summarized in Table 2.
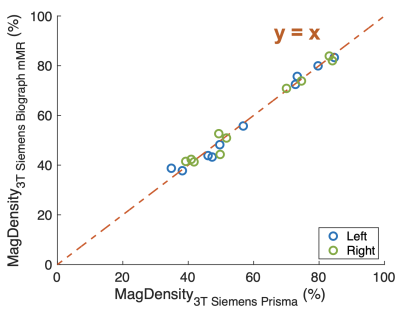
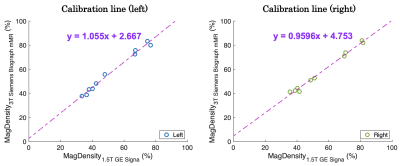
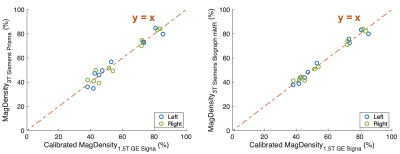
For MagDensity measures across different field strengths and vendors (3T Siemens vs. 1.5T GE), a small systematic bias was observed. Although they remained highly correlated (r > 0.98), larger mean differences were observed (range = 2.5-6.0%). However, this bias can be easily corrected by a linear calibration between the MagDensity measures of 3T Siemens Biograph mMR versus 1.5T GE Signa (no significant difference between the two Siemens scanners). The calibration lines for the left and right breasts are shown in Figure 3. All calibrated Signa MagDensity values were obtained using a leave-one-out cross-validation approach. After the calibration, the observed cross-field/vendor mean differences were within ±0.2%. Pairwise analysis showed no statistically significant difference between the MagDensity measures between 3T Siemens Prisma/Biograph mMR and 1.5T GE Signa (P > 0.05; r > 0.97) (Figure 4). The results are summarized in Table 3.
Discussion
In this study, we assessed the reliability of our previously developed quantitative across various scanners, field strengths, and vendors. The results indicate that MagDensity measures between scanners with the same field strength (3T) and from the same vendor (Siemens) are highly consistent. The measures across two scanners with different field strengths (3T vs. 1.5T) and from two vendors (Siemens vs. GE) are still comparable after a linear calibration.This study has a few limitations that warrant consideration in future research. First, we noticed that the left breasts had a higher mean difference when comparing measures obtained from scanners with different field strengths and vendors. This might be partly due to cardiac motion; further investigation should be conducted to understand this difference. Second, almost all the participants recruited for this study had high BD (greater than 40%). This is due to most of the volunteers being young medical students since the recruitment flyer was posted in a medical school. Future studies will aim to recruit subjects with lower BD.
Conclusion
In this study, we demonstrated that the MR-derived breast density (MagDensity) is comparable across different vendors and field strengths.Acknowledgements
This study was in part supported by the National Institutes of Health (R03CA223052).References
1. Engmann NJ, Scott CG, Jensen MR, et al. Longitudinal changes in volumetric breast density with tamoxifen and aromatase inhibitors. Cancer Epidemiol Biomarkers Prev. 2017;26(6):930-937.
2. Eriksson L, He W, Eriksson M, et al. Adjuvant therapy and mammographic density changes in women with breast cancer. JNCI Cancer Spectr. 2018;2(4):pky071.
3. Ding J, Stopeck AT, Gao Y, et al. Reproducible automated breast density measure with no ionizing radiation using fat-water decomposition MRI. J Magn Reson Imaging. 2018;48(4):971-981.
4. Reeder SB, Pineda AR, Wen Z, et al. Iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL): application with fast spin-echo imaging. Magn Reson Med. 2005;54(3):636-644.
5. Ying J, Cattell R, Zhao T, et al. Two fully automated data-driven 3D whole-breast segmentation strategies in MRI for MR-based breast density using image registration and U-Net with a focus on reproducibility. Vis Comput Ind Biomed Art. 2020;5(1):1-12.
Figures