2726
A comparative study of Kaiser score and BI-RADS in the diagnosis of non-mass enhancement lesions on breast MRI1First affiliated hospital of Wenzhou Medical University, Wenzhou, China, 2University of California, Irvine, California, CA, United States
Synopsis
Keywords: Breast, Breast
A total of 102 malignant and 60 benign non-mass enhancement lesions were analyzed. Two radiologists with 6 (Reader1) and 14 (Reader2) years of experience assigned the BI-RADS category and Kaiser score (KS). KS decreased biopsy or surgery by 20% for Reader 1 and 16.7% for Reader 2 compared with BI-RADS 4-5. The sensitivity, specificity and accuracy were 87.2%, 78.3% and 84.0% for Reader 1, and 85.2%, 83.3% and 84.6% for Reader 2. Using cutoff threshold of KS>4, the specificity of modified KS increased by 6.7% for both readers, increasing the accuracy slightly by 1.7%-2.5% and keeping the same sensitivity.Introduction
The enhanced lesions on breast MRI were divided into focus/foci, mass and non-mass enhancement (NME) 1. NMEs without typical morphology and enhancement features are more difficult to be distinguished between malignant and benign lesions 2. Radiologists assign BI-RADS category on the comprehensive evaluation of the lesion features, which is a complex and experience dependent task 3, 4. Kaiser score (KS), named after Werner A. Kaiser, is a clinical decision-making tool based on five features representing the likelihood of malignant lesions, including root signs, TIC type, lesion margin, internal enhancement pattern, and ipsilateral edema 5, 6. KS is reported to improve the consistency among radiologists, and its diagnostic performance is comparable to BI-RADS, especially for junior or inexperienced radiologists, and could reduce unnecessary breast biopsies 6, 7. Very few studies have focused on the feasibility of KS for NME lesions. The purpose of this study was to compare the diagnostic performance between KS and BI-RADS for NME lesions, and compare the diagnostic efficacy of the two diagnostic methods by radiologists with different diagnostic experience.Methods
A total of 162 NMEs were analyzed, including 102 malignant and 60 benign lesions. MRI protocol consisted of T2WI, T1WI, DWI and DCE. Two radiologists with 6 (Reader 1) and 14 (Reader 2) years of experience assigned the BI-RADS category and KS. KS would be reduced by 4 when the lesions with KS >4 showed an ADC higher than 1.4×10−3 mm2/s and the modified KS would be recorded as KS +. ROC was used to analyze the efficacy of the two diagnostic methods, which was measured by AUC; Youden index was used to determine the optimal cutoff value, and the corresponding sensitivity, specificity and accuracy were calculated. The interobserver agreement between two readers was measured by Cohen’s kappa coefficient.Results
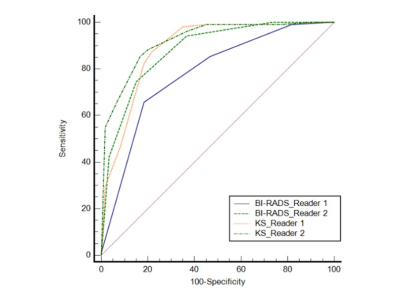
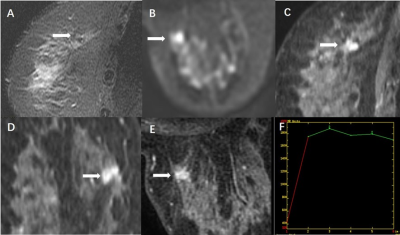
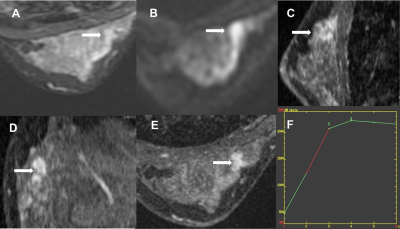
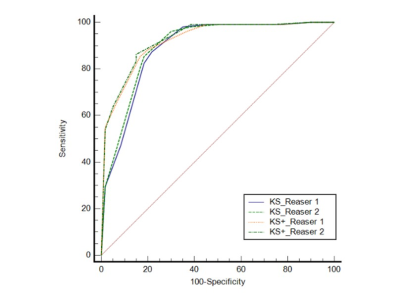
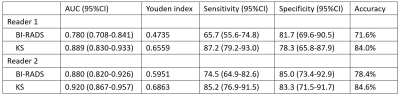
For Reader 1, the AUCs of BI-RADS and KS were 0.780 (95%CI 0.780-0.841) and 0.889 (95%CI 0.830-0.933) (p = 0.003); for Reader 2, those of two methods were 0.880 (95%CI 0.820-0.926) and 0.920 (95%CI 0.867-0.957) (p > 0.05). The AUC of BI-RADS for Reader 2 was significantly higher than that for Reader 1 (p < .001); using KS, Reader 2 markedly improved the diagnostic performance, of whom the AUC was comparable to that of Reader 1 (p > 0.05). The sensitivity, specificity and accuracy were 87.2%, 78.3% and 84.0% for Reader 1, and 85.2%, 83.3% and 84.6% for Reader 2. The AUC, Youden index, sensitivity, specificity and accuracy are summarized in Table 1. ROC curves are shown in Figure 1. Malignant and benign cases are shown in Figure 2 and Figure 3. When using ADC to modify KS and using cutoff threshold of >4, the specificity increased by 6.7% for both readers, with the sensitivity remaining the same and the accuracy slightly increasing. ROC curves of KS and KS+ were shown in Figure 4. The interobserver consistency of KS (κ=0.80, 95%CI 0.74-0.86) was higher than that of BI-RADS (κ=0.56, 95%CI 0.48-0.63) between two readers.Discussion
In this study, we thoroughly compared the diagnostic performance between BI-RADS lexicon and KS for NME from two radiologists with different diagnostic experience, and also evaluated the impact of ADC value on diagnostic efficiency of KS. 35% (21/60) of benign NMEs were diagnosed as KS 5-7 for both readers, which was significantly lower than that of the BI-RADS 4 (81.7% for Reader 1 and 71.7% for Reader 2). However, 21.7% (Reader 1) and 20.0% (Reader 2) of benign NMEs were diagnosed as KS 8-11. It may be due to the fact that NME lesions were more likely to show unclear boundaries, by which radiologists evaluated it as the root sign and would be prone to assign high KS. Although some percentage of NMEs were diagnosed as KS 8-11, KS could still decrease biopsy or surgery by 20% for Reader 1 and 16.7% for Reader 2 compared with BI-RADS 4-5, which was consistent with previous studies 7, 8. The diagnostic performance of KS for Reader 1 was significantly improved compared with that of BI-RADS (AUC was raised from 0.780 to 0.889, p = 0.003), which was comparable to that of Reader 2 (p > 0.05). It indicated that KS evaluation is helpful for inexperienced radiologist to diagnose NME lesions, and its simple flow chart diagnosis can fill the gap in diagnostic effectiveness caused by lack of diagnostic experience. Some researchers proposed that DWI could be combined with tree flow chart scoring to improve diagnostic performance 5. The study demonstrated the similar impact of ADC on KS. Using cutoff threshold of >4, the specificity of modified KS increased by 6.7% for both readers, increasing the accuracy slightly by 1.7%-2.5% and keeping the same sensitivity. But the AUCs of two readers did not show significance before and after modification (0.889 to 0.897 for Reader 1 and 0.920 to 0.926 for Reader 2). In conclusion, the results showed KS assisted junior radiologist dramatically improve the diagnostic performance compared with BI-RADS and shorten the accuracy disparity related to the diagnostic experience compared to senior radiologist. When using ADC value to modify KS, the sensitivity remained the same and the specificity and accuracy slightly increased.Acknowledgements
This work was supported by Incubation Project of First Affiliated Hospital of Wenzhou Medical University (No. FHY2019085), and Wenzhou Science & Technology Bureau (No. Y20210232).References
1. Edwards SD, Lipson JA, Ikeda DM, et al. Updates and revisions to the BI-RADS magnetic resonance imaging lexicon. Magn Reson Imaging Clin N Am. 2013;21(3):483-493.
2. Torous VF, Resteghini NA, Phillips J, et al. Histopathologic Correlates of Nonmass Enhancement Detected by Breast Magnetic Resonance Imaging. Arch Pathol Lab Med. 2021;145(10):1264-1269.
3. Sohns C, Scherrer M, Staab W, Obenauer S. Value of the BI-RADS classification in MR-Mammography for diagnosis of benign and malignant breast tumors. Eur Radiol. 2011;21(12):2475-2483.
4. Marino MA, Riedl CC, Bernathova M, et al. Imaging Phenotypes in Women at High Risk for Breast Cancer on Mammography, Ultrasound, and Magnetic Resonance Imaging Using the Fifth Edition of the Breast Imaging Reporting and Data System. European Journal of Radiology. 2018;106:150-159.
5. Dietzel M, Baltzer PAT. How to use the Kaiser score as a clinical decision rule for diagnosis in multiparametric breast MRI: a pictorial essay. Insights Imaging. 2018;9(3):325-335.
6. Marino MA, Clauser P, Woitek R, et al. A simple scoring system for breast MRI interpretation: does it compensate for reader experience? Eur Radiol. 2016;26(8):2529-2537.
7. Woitek R, Spick C, Schernthaner M, et al. A simple classification system (the Tree flowchart) for breast MRI can reduce the number of unnecessary biopsies in MRI-only lesions. Eur Radiol. 2017;27(9):3799-3809.
8. Milos RI, Pipan F, Kalovidouri A, et al. The Kaiser score reliably excludes malignancy in benign contrast-enhancing lesions classified as BI-RADS 4 on breast MRI high-risk screening exams. Eur Radiol. 2020;30(11):6052-6061.
Figures