2700
SAR Simulations with a Poseable Numerical Body Model for 3T MRI of Straight & Flexed Knee: First Results1Radiology, NYU Grossman School of Medicine, New York, NY, United States, 2Center for Advanced Imaging Innovation and Research (CAI2R), New York University, New York, NY, United States
Synopsis
Keywords: Safety, Safety
Although recent developments in flexible coils have allowed for imaging of the knee in a flexed or straight position, simulations for safety assessment are typically performed with both legs straight. Here we show first results of SAR simulations with both legs straight versus knee flexed with fields normalized as if imaging the knee that is changing position. Results indicate a decrease in maximum 10g SAR when the knee being imaged is flexed.Introduction
Recently, close-fitting flexible receive-only knee array coils have been developed to both improve SNR compared to larger rigid coils and allow for MRI of the knee in different positions1,2. Because simulations to ensure MR safety are typically performed with both legs straight there may be concern about effects of different leg positions on maximum local SAR values. Here we use numerical simulations to perform a first examination of implications on SAR for MRI with the imaged knee bent versus with both legs straight.Methods
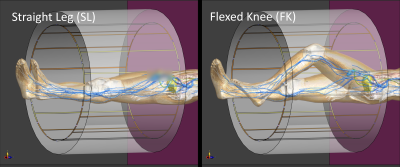
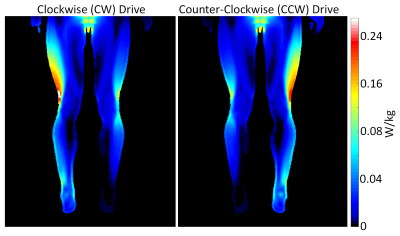
Numerical models of a human body (Duke3) positioned with the left knee in the center (longitudinally) of a 16-rung high-pass birdcage coil (radius 325mm, length 600mm, shield radius 400mm) when both legs were straight and when the left knee was flexed (Figure 1) were developed using commercially-available simulation software (Sim4Life, ZMT, Zurich) and its internal implementation of the BirdcageBuilder tool4. The coil was tuned to 128MHz and driven in quadrature across two capacitors 90 degrees apart (both beneath the table and 45 degrees from horizontal or vertical) to produce both clockwise (CW) and counter-clockwise (CCW) dominant circularly-polarized RF magnetic fields (rotational direction defined as looking from head-to-foot direction), which could be pertinent to imaging in systems with $$$B_0$$$ oriented in the foot-head vs. head-foot direction or – given the near mirror symmetry of the SAR distributions (Figure 2) – with either the left knee or right knee flexed.For both CW and CCW drive configurations and both Straight Leg (SL) and Flexed Knee (FK) body positions, $$$B_1$$$ field and 10g-averaged SAR distributions were exported for use in Matlab (The Mathworks, Natick). For both CW and CCW drives, 10g SAR distributions were normalized to the square of the dominant circularly-polarized component of the RF magnetic field $$$|B_1^+|$$$ at the center of the left knee when the left knee was both straight and flexed so that the femur was 30 degrees from horizontal and the heel remained on the patient table.
Results
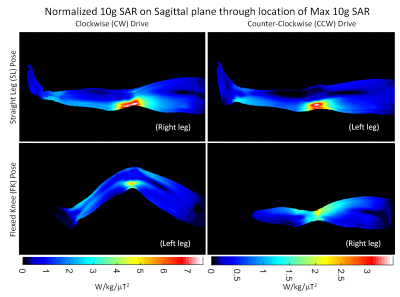
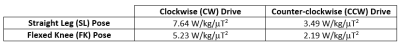
Figure 3 shows the normalized 10g SAR distribution on the sagittal plane passing through the location of maximum 10g SAR for both body poses in both drive configurations, and with the same color scale range used for a given drive configuration. Table 1 shows the numerical value of normalized maximum 10g SAR in all four cases. As indicated above, the SAR values are normalized as if the same MR sequence were to be used on the left knee while in straight and flexed positions. For both drive configurations, the maximum local 10g SAR is lower when the left knee is flexed than when both legs are straight.Discussion
In these initial simulations, maximum 10g SAR decreases when one knee is bent versus when both legs are straight. While in our simulations only the left knee is bent, we expect that due to near-mirror symmetry of the SAR patterns when the birdcage coil is driven with opposite polarization, the observation that this effect occurs for either drive configuration could be applied to either opposite $$$B_0$$$ directions or to imaging of the opposite knee in either position. To increase certainty of this trend, it will be necessary to explicitly simulate situations with either and both knees flexed, including a larger portion of the body model extending out of the birdcage coil, and in additional body models. Meanwhile it appears there is no need for concern about a significant increase in maximum local SAR when imaging with one knee flexed.Acknowledgements
This work has benefited from funding by the National Institutes of Health through NIH P41 EB017183 (CAI2R) and discussions with Jan Paska and Giuseppe Carluccio.
References
1. Siddiq SS, Ho J, Wang D, Walczyk J, Lakshmanan K, Brown R. Wearable knee receive array coil for imaging at different flexion angles. Proc. 2021 ISMRM, p. 0132
2. Wang B, Siddiq SS, Walczyk J, et al. A flexible MRI coil based on a cable conductor and applied to knee imaging. Sci Rep 2022;12:15010 doi: 10.1038/s41598-022-19282-6.
3. Gosselin, et al. Development of a new generation of high-resolution anatomical models for medical device evaluation: the Virtual Population 3.0, Physics in Medicine and Biology, 59(18):5287-5303, 2014.
4. Chin C-L, Collins CM, Li S, Dardzinski BJ, Smith MB. BirdcageBuilder: Design of specified-geometry birdcage coils with desired current pattern and resonant frequency. Concepts Magn. Reson. 2002;15:156–163 doi: 10.1002/cmr.10030.
Figures