2656
Elevated Carotid Pulse Wave Velocity is associated with Cognitive Impairment and Brain Amyloid Deposition
Jianing Tang1,2, Elizabeth Joe3, Helena Chui3, and Lirong Yan2,3
1Biomedical Engineering, Northwestern University, Evanston, IL, United States, 2Radiology, Northwestern University, Evanston, IL, United States, 3Department of Neurology, University of Southern California, Los Angeles, CA, United States
1Biomedical Engineering, Northwestern University, Evanston, IL, United States, 2Radiology, Northwestern University, Evanston, IL, United States, 3Department of Neurology, University of Southern California, Los Angeles, CA, United States
Synopsis
Keywords: Alzheimer's Disease, Blood vessels
Increasing evidence suggests that vascular compliance could offer valuable insights into the pathology of Alzheimer’s diseases. Recently, carotid pulse wave velocity (cPWV) between internal carotid artery and common carotid artery has been successfully measured by a fast single-slice oblique-sagittal PC-MRI technique. In this study, we evaluated the role of cPWV in brain amyloid deposition and cognitive decline in an aged cohort. The results showed that greater cPWV was associated with cognitive decline and amyloid pathology. Our findings suggest elevated cPWV may affect amyloid clearance in brain, leading to cognitive impairment. cPWV could be a potential sensitive imaging marker of AD.Introduction
Accumulative evidence suggests that vascular dysfunction contributes to the pathology of Alzheimer’s disease (AD). Arterial stiffness or vascular compliance is one of the earliest markers of vascular dysfunction1. Arterial stiffening induces the transmission of excessive pulsations into the downstream microvasculature, resulting in microcirculation dysfunction as well as vascular inflammation. Pulse wave velocity (PWV) is an established surrogate of arterial stiffness. PWV is commonly used to access the arterial stiffness of the central and peripheral arteries measured by ultrasound. To date, there remains limited work to non-invasively assess the arterial stiffness in the brain, which could be closely linked to AD pathology. Transcranial Doppler (TCD) has been used to record the arterial pulse waves at the middle cerebral artery (MCA) and internal carotid artery (ICA). However, this procedure is operator-dependent, time-consuming, and contingent upon the availability of an acoustic window, which is limited in some elderly individuals. Recent work has introduced a fast and robust MRI method to measure carotid PWV (cPWV) by simultaneously acquiring multiple arterial velocity waveforms along the common carotid artery (CCA) and ICA using a single-slice oblique-sagittal phase-contrast MRI (OS PC-MRI)2,3. The present study aims to evaluate cPWV measured by OS PC-MRI as a sensitive vascular marker of AD by studying the association of cPWV with cognitive performance and amyloid pathology.Methods
Participants and clinical assessments:Twenty-three elderly participants (13 female, 72.6 ± 7.1 years) were enrolled in the study. All participants provided written informed consent prior to participating in the study. Cognitive assessments were conducted, where all 23 participants had Clinical Dementia Rating (CDR), 21 received Mini-Mental State Exam (MMSE) and 17 received Montreal Cognitive Assessment (MoCA). 14 out of the 23 participants underwent PiB-PET scans to assess amyloid pathology.
MRI experiments:
The MRI experiments were conducted on a 3T MRI scanner (Magneton Prisma, Siemens Healthcare, Erlangen, Germany) using a 20-channel head coil. A 2min TOF MRI was performed to localize carotid arteries including CCA and ICA. The 3D MR angiogram was reformatted to determine an oblique slice to maximally cover both CCA and ICA segments as shown in Figures 1a and b. A single-slice retrospective gated 2D OS PC-MRI with a single in-plane velocity encoding (CCA to ICA) was performed on each participant to simultaneously acquire blood velocity waveforms in the CCA-ICA segment. Imaging parameters were spatial resolution=1x1x1mm3, VENC=80cm/s, TE/TR=4.32/14.22ms, flip angle=10°, real temporal resolution=14.22ms, number of phases=70-90, scan time was 1 to 2min depending on the heart rate.
Image processing and statistical analysis
A reference waveform was calculated as the average of velocity waveforms obtained from all axial locations along ICA-CCA. The transit time between each waveform and the reference waveform was calculated using time-to-foot (TTF) method2. cPWV was calculated as the inverse slope of the line fitted to the transit time versus distance along the vessel (Figure 1c).
A One-sample Kolmogorov-Smirnov test was performed on each dataset (PWV, MoCA, MMSE, age) to determine whether that data set follows a normal distribution. According to the results of the normality test, the correlations between cPWV vs cognitive measures and amyloid status were calculated across subjects using Pearson or Spearman's correlation coefficients. Age, gender, and education were considered as covariances in the analysis.
Results and Discussion
Table 1 lists the demographics and clinical assessment information of the participants in the study. Figures 2a and b show the scatter plots of cPWV with MoCA and MMSE across subjects, respectively. cPWV showed significant negative correlations with both MoCA and MMSE (cPWV vs. MoCA: r = -0.45, p = 0.07; cPWV vs. MMSE: r = -0.74, p < 0.001), and the correlations remained significant after controlling for age, gender, years of education (cPWV vs. MoCA: r = -0.64, p = 0.02; cPWV vs. MMSE: r = -0.75, p < 0.001). The participants were further separated into two groups (CRD=0: n=12; CDR>=0.5: n=11) based on their CDR scores as clinical cognitive assessment. Consistent with the above findings, cPWV values were significantly higher in the group with CDR>= 0.5 without and with correcting for age, sex, and educational level (p=0.0019, p=0.015). These results provide convergent evidence that elevated cPWV is associated with cognitive decline. 7 of 14 participants who underwent PiB PET scans were diagnosed with amyloid positive. There was a strong association between cPWV and amyloid pathology (p=0.038), further suggesting cPWV may be closely linked to amyloid pathology in AD.Conclusion
This study has demonstrated that elevated carotid PWV is associated with cognitive impairment and amyloid pathology in elderly adults. This study could shed more light on the vascular contribution to AD pathology. To our best knowledge, this is the first to study the association between amyloid pathology and intracranial arterial stiffness, suggesting intracranial arterial stiffening affects amyloid clearance in the brain, leading to amyloid deposition in the brain. Compared to TCD, OS PC-MRI is a fast (1-2 minutes) and reliable MRI method for cPWV measurement. cPWV measured using 2D OS PC-MRI could be a sensitive imaging marker of Alzheimer’s disease. Future studies will be carried out to study the regional associations between amyloid burden and cPWV.Acknowledgements
This work is supported by grants from NIH R01NS118019, RF1AG072490, and BrightFocus Foundation A20201411S.References
1. Parittotokkaporn S, de Castro D, Lowe A, Pylypchuk R. Carotid Pulse Wave Analysis: Future Direction of Hemodynamic and Cardiovascular Risk Assessment. JMA J. 2021;4(2):119-128. doi:10.31662/jmaj.2020-0108
2. Heidari Pahlavian S, Cen SY, Bi X, Wang DJJ, Chui HC, Yan L. Assessment of carotid stiffness by measuring carotid pulse wave velocity using a single-slice oblique-sagittal phase-contrast MRI. Magn Reson Med. 2021;86(1):442-455. doi:10.1002/mrm.28677
3. Tang J, Pahlavian SH, Chui H, Yan L, Evaluation of the robustness of carotid pulse wave velocity measurement using a single-slice oblique-sagittal phase-contrast MRI. In: Proc 28th Annual Meeting ISMRM, London 2022.
Figures
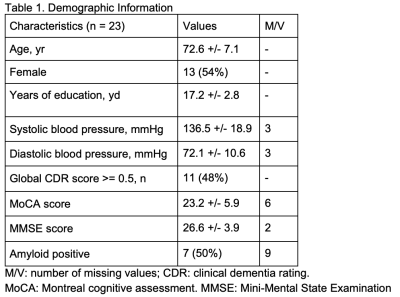
Table 1. Demographic Information
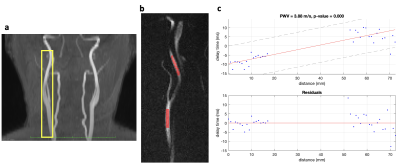
Figure 1. a. 3D time-of-flight angiogram. A yellow box indicates the imaging plane of OS PC-MRI covering the ICA and CCA segments; b CCA-ICA ROI selection; c the scatter plots of transit time (or delay time) versus vessel distance and calculated cPWV value using the ROI in figure b.
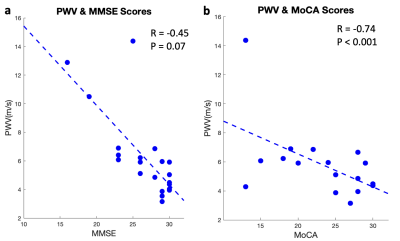
Figure 2. Scatter plots of PWV values with MoCA scores (a) and MMSE scores (b) across subjects. Correlation coefficient of PWV vs. MoCA is -0.45, p = 0.07 (Spearman); Correlation coefficient of PWV vs. MMSE is -0.6455, p = 0.0015 (Spearman).
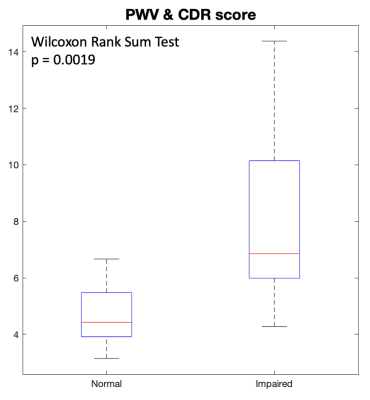
Figure 3. Box plot between the participants with normal cognition (CDR=0) and with cognitive impairment (CDR>=0.5). Significant difference (p = 0.0019) in cPWV was observed between the two groups.
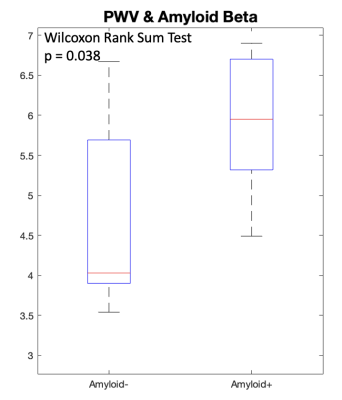
Figure 4. Box plot between participants with amyloid negative and amyloid positive. Significant differences (p=0.038) were observed between the two groups.
DOI: https://doi.org/10.58530/2023/2656