2591
Evaluation of the peripheral nerves of the knee using Double-Echo Steady-State MRI at 7T1The first affiliated hospital ofArmy Medical University, Chongqing, China, 2The first affiliated hospital, Army Medical University, Chongqing, China, 3MR Collaborations, Siemens Healthineers Ltd., Chengdu, China
Synopsis
Keywords: MSK, Nerves, 7T, DESS, peripheral nerves
This study investigated the feasibility of DESS sequence to assess the knee peripheral nerve structures in healthy subjects and patients. The results showed that the nerve imaging quality of DESS sequence was superior to PD sequence in healthy adults. Further, only the isotropic 3D-DESS protocol could clearly visualize the distal peroneal nerve branches and their anatomical course. In patient with peripheral nerves damages, combining the PD and DESS imaging could provide more pathological and anatomical information about the knee peripheral nerve. This suggests that DESS sequence can reliably image the knee peripheral nerves and effectively provide precise knowledge about it.Introduction
Injuries in the peripheral nerves of the knee are commonly encountered and lead to dysfunction in the lower limb in the clinic. The peroneal nerve (PN), tibial nerve (TN), and saphenous nerve (SN) are the main peripheral nerves of the knee, which cannot be reliably visualized on 3T MRI[1]. These nerves are vulnerable to tractions and compressions by external forces[2]. Injuries to these nerves can cause pain, numbness, and weakness in the affected legs[3]. Previous research has shown the feasibility of imaging the sciatic nerve and fascicular structures at 7T MR using the DESS sequence[4], which provided high soft tissue contrast and superior spatial resolution. However, so far, the application of the DESS sequence in imaging of the peripheral nerves of the knee has not been fully studied. Hence, this study aims to evaluate the potential of the DESS sequences at 7T MR for assessing the detailed structures of the peripheral nerve of the knee.Methods
Twenty-two healthy subjects (22 right knee joints) and one patient (one right knee joint) underwent MR scans at 7T (MAGNETOM Terra, Siemens Healthcare, Erlangen, Germany) with a 28-channel knee coil. Scanning protocols (Table 1) included axial Proton Weighted (PD) images and two three-dimensional double-echo steady-state (3D-DESS) sequences with different resolutions: sagittal DESS-A images for 3D structural evaluation (reconstructed to axial plane) and axial DESS-B images with high in-plane resolution for the nerve fascicles assessment. For comparison, all images were evaluated in the axial plane. The quality of nerve images in different sequences was evaluated by two radiologists with a 3-grade scale[5]. The signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) of the nerves to surrounding fat tissue at the popliteal fossa level were measured.Results
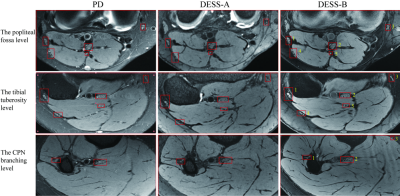
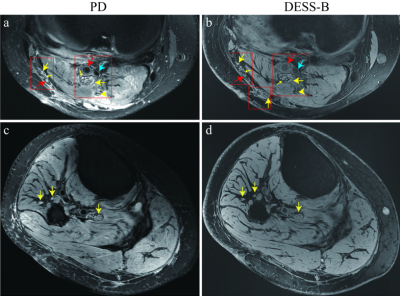
In general, the PD images provided fair details for the peripheral nerves compared to DESS images. DESS-A protocol provided superior delineation of the peroneal nerve (PN), and DESS-B protocol with 0.1x0.1mm2 in-plane resolution provided excellent image quality for depicting the tibial nerve (TN) and saphenous nerve (SN). A good agreement of subjective scores for image quality was obtained, with a κ value around 0.65 to 1. The subjective scores, SNR and CNR of the three protocols were summarized in Table 2. The SNR and CNR measurements of the saphenous nerve were not performed due to the poor display on the DESS-A protocol. For visualization of the detailed nerve structures, the distal PN branches could be better depicted on DESS-A images, while DESS-B images provided fine structures of the small nerve branches for the TN and SN (Fig. 1, Fig. 2). The representative images of a patient with peripheral nerves damages caused by trauma are shown in Figure 3. The PD imaging showed markedly swollen TN and PN with enhanced signal and thickening of the nervous tracts and epineurium. Thickened tibial and peroneal individual nerve fascicles and muscular branches of the TN and the lateral sural cutaneous nerve were clearly observed on DESS-B images.Discussions and conclusions
Our study demonstrated the feasibility of knee peripheral nerves visualization at 7T MR using high resolution DESS sequences. Though PD sequence was sensitive to inflammation and infarction of the peripheral nerves lesion, DESS sequences provided much sharper image quality and enabled delineation of small nerve branches. The use of 3D-DESS images of the peripheral nerves and their branches of the human knee joint is of great value for the guidance of surgery and the diagnosis of nerve-related entrapment syndrome.The DESS sequences have the potential to provide precise assessments of the peripheral nerves of the knee. Combining the DESS sequences with the PD sequence could provide more valuable information for the diagnosis of knee peripheral nerve diseases and assisting the preparation for surgery.
Acknowledgements
This study has received funding from the Chongqing Science and Technology Commission, China (No. cstc2019jscx-msxmX0221).References
1. Kavolus, J.J., et al., Saphenous Nerve Block From Within the Knee Is Feasible for TKA: MRI and Cadaveric Study. Clin Orthop Relat Res, 2018. 476(1): p. 30-36.
2. Chang, K.V., et al., Ultrasound Imaging for the Cutaneous Nerves of the Extremities and Relevant Entrapment Syndromes: From Anatomy to Clinical Implications. J Clin Med, 2018. 7(11).
3. Fisse, A.L., et al., Cross-sectional area reference values for peripheral nerve ultrasound in adults: A systematic review and meta-analysis-Part II: Lower extremity nerves. Eur J Neurol, 2021. 28(7): p. 2313-2318.
4. Sveinsson, B., et al., Feasibility of simultaneous high-resolution anatomical and quantitative magnetic resonance imaging of sciatic nerves in patients with Charcot-Marie-Tooth type 1A (CMT1A) at 7T. Muscle Nerve, 2022. 66(2): p. 206-211.
5. Galley, J., et al., High-resolution in vivo MR imaging of intraspinal cervical nerve rootlets at 3 and 7 Tesla. Eur Radiol, 2021. 31(7): p. 4625-4633.
6. Pazahr, S., D. Nanz, and R. Sutter, 7 T Musculoskeletal MRI: Fundamentals and Clinical Implementation. Invest Radiol, 2022.
Figures
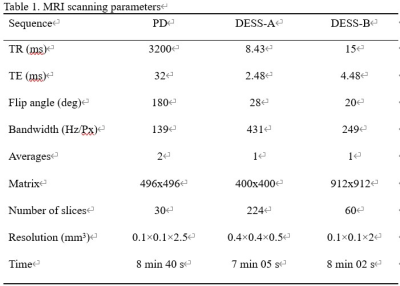

Table 2. Subjective assessment of the peripheral nerve imaging
PN peroneal nerve; TN tibial nerve; SN saphenous nerve