2569
Effect of general anesthesia on cerebral blood flow measured by Arterial Spin Labeling: A retrospective study
Thomas Lindner1, Monika Huhndorf2, Christine Eimer3, Tobias Becher3, Hajrullah Ahmeti4, Olav Jansen2, Michael Synowtiz4, Michael Helle5, and Stephan Ulmer2,6
1UKE Hamburg, Hamburg, Germany, 2Department of Radiology and Neuroradiology, University Hospital Schleswig-Holstein, Kiel, Germany, 3Department of Anesthesia, University Hospital Schleswig-Holstein, Kiel, Germany, 4Department of Neurosurgery, University Hospital Schleswig-Holstein, Kiel, Germany, 5Philips Gmbh Innovative Technologies, Hamburg, Germany, 6neurorad.ch, Zurich, Switzerland
1UKE Hamburg, Hamburg, Germany, 2Department of Radiology and Neuroradiology, University Hospital Schleswig-Holstein, Kiel, Germany, 3Department of Anesthesia, University Hospital Schleswig-Holstein, Kiel, Germany, 4Department of Neurosurgery, University Hospital Schleswig-Holstein, Kiel, Germany, 5Philips Gmbh Innovative Technologies, Hamburg, Germany, 6neurorad.ch, Zurich, Switzerland
Synopsis
Keywords: Arterial spin labelling, Brain, Anesthesia
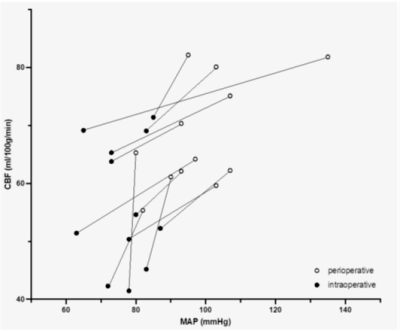
In this study, we non-invasively evaluated the change in cerebral blood flow (CBF) and correlation with mean arterial pressure (MAP) before and during anesthesia using Arterial Spin Labeling. It could be shown that both CBF and MAP are reduced comparing the awake and anesthesia-induced state in patients.Introduction
The human brain needs a continuous supply of oxygen and nutrients to fulfill its needs of high energy consumption. In the healthy brain, this is maintained by autoregulation of cerebral blood flow (CBF) which ensure a constant supply of blood across a dynamic range of blood pressures. Brain pathologies, drugs and anesthesia however can impede this autoregulation. Arterial Spin Labeling (ASL) is a well-known technique for the non-invasive evaluation of CBF [1]. ASL has already been used in a variety of clinical questions, but the effect of anesthesia-induced CBF changes has only been evaluated in a small group of cases yet [2]. The aim of the present study is to evaluate anesthesiologically induced peri- and intraoperative changes in CBF during neurosurgical interventions.Materials and Methods
The patient collective consisted of 12 patients with intracranial tumors who underwent neurosurgery. Next to the clinically used structural MRI sequences, pseudo continuous Arterial Spin Labeling (PCASL) was used to evaluate CBF. Image acquisition was performed perioperatively in the awake state and intraoperatively under general anesthesia and mechanical ventilation. Perioperative scanning was performed either on a 3T or 1.5T Achieva scanner and intraoperative MRI on a 1.5T Intera scanner. All from Philips Healthcare, Best, The Netherlands. Scan parameters of ASL were: 2D EPI PCASL with 3.6x3.5mm² voxel size consisting of 16 slices with 5mm thickness and a gap of 1mm. TR/TE: 2616/13, EPI factor: 39, field-of-view: 224x224x95mm, matrix size: 64x64, flip angle: 90°. Label/control pairs were 20 for 3T and 30 for 1.5T perioperatively and 40 pairs intraoperatively. An additional T2 scan with the same slice thickness and number of slices was performed as anatomical reference. CBF was evaluated on the healthy (non-tumorous) hemisphere by calculating a hemisphere-average CBF value using manual regions of interest. Recorded physiological parameters include mean arterial blood pressure (MAP), blood oxygen saturation (SaO2), heart rate (HR) and end-tidal carbon dioxide (etCO2) (Table 1).Results and Discussion
MAP varied between 80 and 135 mmHg peri- and 62-90 mmHg intraoperative. CBF was 68.3 ± 9.3 ml/100g/min peri- and 56.4 ± 10.9 ml/100g/min. All values are presented in Table 1. In all patients, both MAP and CBF were reduced under anesthesia (Figure 1). Intraindividual comparison of the patients showed a reduction in CBF between 9.32% and 36.51%. No statistically significant correlations between MAP and CBF could be found (neither peri-, nor intraoperative).Conclusion
ASL is a potent method to non-invasively investigate changes in brain perfusion induced by anesthesia. The main finding of this study is that in all patients both the MAP and CBF are reduced under the influence of anesthetic drugs, but do not fall under the ischemic threshold. This can be seen as a preliminary application of ASL to monitor and investigate drug-induced CBF changes in certain populations.Acknowledgements
No acknowledgement found.References
[1] Alsop DC, Detre JA, Golay X, et al. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med. 2015;73(1):102-116. doi:10.1002/mrm.25197
[2] Venkatraghavan L, Poublanc J, Bharadwaj S, Sobczyk O, Crawley AP, Mandell DM, Mikulis DJ, Fisher JA. Noninvasive Measurement of Cerebral Blood Flow Under Anesthesia Using Arterial Spin Labeling MRI: A Pilot Study. J Neurosurg Anesthesiol. 2016 Oct;28(4):331-6. doi: 10.1097/ANA.0000000000000231. PMID: 26397237.
DOI: https://doi.org/10.58530/2023/2569