2558
Differentiating Benign from Malignant Breast Lesions and Molecular Subtypes Using MRI with a Continuous-Time Random-Walk Diffusion Model1Department of Radiology, Shandong Provincial Qianfoshan Hospital, Shandong University, Shandong, China, Jinan, China, 2Department of Radiology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital,Shandong, China, Jinan, China, 3Department of Radiology, The First College of Clinical Medicine, Shandong University of Traditional Chinese Medicine, Shandong, China, Jinan, China, 4MR Collaboration, Central Research Institute, United Imaging Healthcare, Shanghai, China, Shanghai, China, 5Department of Breast Surgery, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital,Shandong, China, Jinan, China
Synopsis
Keywords: Breast, Diffusion/other diffusion imaging techniques
Accurately differentiating breast cancer is crucial for clinical treatment. However, it is challenging due to the high heterogeneity of breast cancer. This study used a continuous-time random-walk (CTRW) diffusion model to characterize breast lesions and their molecular subtypes. The malignant lesions had significantly lower ADC, Dm, and α values than benign lesions. Significant differences were also found between luminal A and triple-negative groups in parameter β. And the combination of CTRW parameters yielded better performance in classifying breast cancer than ADC. Therefore, this study highlights that the CTRW parameters are superior to ADC in distinguishing breast lesions and molecular subtypes.Introduction
Breast cancer is the most common malignancy among females and can be classified into four subtypes: triple-negative (TN), luminal A, luminal B, and human epidermal growth factor 2-positive (HER2-positive)1. Accurately differentiating malignant from benign lesions and identifying molecular subtypes are crucial for clinical treatment2. However, due to the high heterogeneity of breast cancer3, it is difficult to classify different breast lesions, which makes customized treatment difficult.Previous studies had indicated that diffusion-weighted imaging (DWI) can improve overall diagnostic accuracy, sensitivity, and specificity of breast cancer detection4. The apparent diffusion coefficient (ADC) derived from DWI had been proven useful in the characterization of breast cancer5. However, breast lesions conform to a non-Gaussian distribution process, and the ADC cannot well describe non-Gaussian diffusion behavior of water molecules in tissue and lacks specific parameters to reflect the complexity of the tumor microenvironment6.
Recently, a continuous-time random-walk (CTRW) diffusion model had been introduced and applied to brain diseases7,8,9. The CTRW model provides two new parameters, α, and β, for characterizing temporal and spatial diffusion heterogeneities, respectively7,8. Together with the anomalous diffusion parameter Dm, the three parameters can assess different aspects of complex microstructure and different dimensions of heterogeneity in tumor tissues.
However, the effectiveness of the CTRW model in diagnosing breast lesions and identifying molecular subtypes is still unclear. Therefore, the current exploratory study aimed to investigate the value of using a CTRW diffusion model to distinguish between benign and malignant breast lesions and to differentiate among the molecular subtypes.
Methods
MRI acquisition:Sixty-two patients with histopathologically confirmed breast lesions (53 malignant and 9 benign breast lesions) were enrolled in this prospective study (Table 1). MRI examinations were performed with a 3.0T scanner (uMR 790, United Imaging Healthcare, Shanghai, China) to obtain 16 b-values (0, 10, 20, 30, 50, 70, 100, 150, 200, 400, 800, 1200, 1500, 2000, 2500, 3000 s/mm2) DWI.
Image analysis:
The CTRW model was fitted by the following equation7,8:
S / S0 = Eα [-(bDm)β]
where Dm is an anomalous diffusion coefficient, α and β are parameters related to temporal and spatial diffusion heterogeneity, respectively, and Eα is a Mittag-Leffler function.
The ADC derived from a DWI model was calculated for comparison using the following equation:
S / S0 = eb*ADC
where S is the signal intensity acquired at b-values=400, 800 s/mm2, S0 is the signal intensity in the voxel with b-values=0 s/mm2.
Regions of interest (ROIs) were drawn manually on the slice with the largest tumor area (cystic or necrotic areas were excluded) on each diffusion image with b-value = 1200 s/mm2. These ROIs were then copied onto the parameter maps (Dm, α, β, and ADC maps).
Statistics:
The CTRW parameters (Dm, α, and β) and ADC were compared between benign and malignant lesions and among the molecular subtypes by Mann–Whitney U-test. Furthermore, binary logistic regression and receiver operating characteristic (ROC) curve analysis was used to evaluate the diagnostic performance of the individual ADC or CTRW parameters and their combinations. P-value <0.05 was considered as significant difference.
Result
The parameters, Dm, α, ADC were significantly lower (P=0.023, 0.016, 0.018, respectively) in the malignant (1.019±0.295 μm/mm2, 0.846±0.094, 1.082±0.293 μm/mm2, respectively) than benign (1.413±0.295 μm/mm2, 0.925±0.072, 1.377±0.485 μm/mm2, respectively) lesions (Figure 1, Table 2). And the combination of α and β produced the best area under curve (AUC, 0.761) and specificity (84.1%) (Table 3).For distinguishing molecular subtypes, significant differences were found when comparing the parameter β in the luminal A and TN groups(p=0.031). And the luminal A had significantly higher Dm (p=0.008) and ADC (p=0.010) than luminal B (Figure 2, Table 2). Furthermore, for the classification of TN and luminal A subtypes, the combination of Dm, α, and β performed the highest AUC (0.874), sensitivity (82.6%), and specificity (88.9%) (Table 3).
Discussion
The current study showed that the Dm, α, ADC were significantly lower in the malignant than benign lesions. Prior studies8,9,10 suggested that the parameter α had been associated with temporal diffusion heterogeneity. A smaller α in the malignant lesions suggested that the more variable time for the diffusing water molecules to move through heterogeneous environment was need, and the diffusion process was more inhomogeneous temporally. The Dm and ADC were sensitive to tissue cellularity, lower ADC and Dm showed the denser cellularity and more inhomogeneous microenvironment in malignant lesions11,12.Several studies had indicated that the CTRW model can improve diagnostic accuracy over ADC in differentiating brain tumor grades because of their ability to probe diffusion heterogeneities 11,12. The present study also demonstrated that the CTRW parameters (Dm, α, β) naturally include tissue cellularity and heterogeneity in space and time domains, and combining the CTRW parameters could provide complementary tissue properties in describing complex lesions.
Although no significant difference was observed for distinguishing benign from malignant lesions by a single parameter β in this study, its combination with parameter α showed better specificity than single parameter α. This suggested that β may be useful in enhancing the value of α in identifying and quantifying microenvironmental heterogeneity in breast cancer.
In conclusion, our findings highlight the CTRW parameters are superior to conventional ADC in distinguishing breast lesions and differentiating among the molecular subtypes.
Acknowledgements
NOReferences
1. Fan, M., He, T., Zhang, P., Cheng, H., Zhang, J., Gao, X., & Li, L. Diffusion-weighted imaging features of breast tumours and the surrounding stroma reflect intrinsic heterogeneous characteristics of molecular subtypes in breast cancer. NMR in Biomedicine, 2018 31(2), 1–11.2. Iima, M., et al. Intravoxel incoherent motion and quantitative non-Gaussian diffusion MR imaging: Evaluation of the diagnostic and prognostic value of several markers of malignant and benign Breast lesions. Radiology, 2018 287(2). 432–441.
3. You C, Li J, Zhi W, Chen Y, Yang W, Gu Y, Peng W. The volumetric-tumour histogram-based analysis of intravoxel incoherent motion and non-Gaussian diffusion MRI: association with prognostic factors in HER2-positive breast cancer. J Transl Med. 2019 Jul 2;17(1):182.
4. Maltez de Almeida JR, Gomes AB, Barros TP, Fahel PE, de Seixas Rocha M. Subcategorization of Suspicious Breast Lesions (BI-RADS Category 4) According to MRI Criteria: Role of Dynamic Contrast-Enhanced and Diffusion-Weighted Imaging. AJR Am J Roentgenol. 2015 Jul;205(1):222-31.
5. You, C., et al. The volumetric-tumour histogram-based analysis of intravoxel incoherent motion and non-Gaussian diffusion MRI: Association with prognostic factors in HER2-positive breast cancer. Journal of Translational Medicine, 2019 17(1)1–11.
6. Iima, M. et al. Quantitative Non-Gaussian Diffusion and Intravoxel Incoherent Motion Magnetic Resonance Imaging. Investigative Radiology, 2015 50(4), 205–211.
7. Ingo, C., et al. On random walks and entropy in diffusion-weighted magnetic resonance imaging studies of neural tissue. Magnetic Resonance in Medicine, 2014 71(2):617–627.
8. Karaman MM, Zhang J, Xie KL, Zhu W, Zhou XJ. Quartile histogram assessment of glioma malignancy using high b-value diffusion MRI with a continuous-time random-walk model. NMR Biomed. 2021 Apr;34(4):e4485.
9. Karaman MM, Sui Y, Wang H, Magin RL, Li Y, Zhou XJ. Differentiating low- and high-grade pediatric brain tumors using a continuous-time random-walk diffusion model at high b-values. Magn Reson Med. 2016 Oct;76(4):1149-57.
10. Zhang J, Weaver TE, Zhong Z, Nisi RA, Martin KR, Steffen AD, Karaman MM, Zhou XJ. White matter structural differences in OSA patients experiencing residual daytime sleepiness with high CPAP use: a non-Gaussian diffusion MRI study. Sleep Med. 2019 Jan;53:51-59.
11. K. Sun, X. Chen, W. Chai, et al., Breast cancer: diffusion kurtosis MR imaging-di- agnostic accuracy and correlation with clinical pathologic factors, Radiology 2015 277 46–55.
12. S. Suo, K. Zhang, M. Cao, et al., Characterization of breast masses as benign or malignant at 3.0T MRI with whole-lesion histogram analysis of apparent diffusion coefficient, J. Magn. Reson. Imaging: 2016 JMRI 43 894–902.
Figures
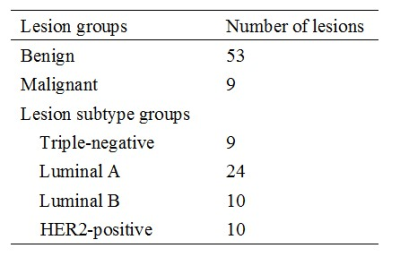
Table 1. Clinical data for patients enrolled in this study, including benign and malignant status, molecular subtypes.
Abbreviations: HER2= human epidermal growth factor receptor 2.
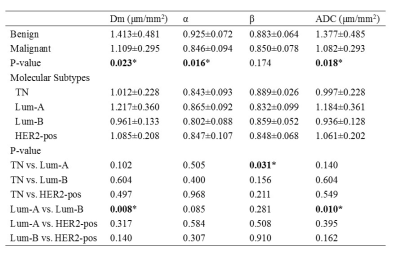
Table 2. Comparison of Dm, α, β, and ADC among benign from malignant breast lesions and different molecular subtypes.
Abbreviations: TN=triple-negative; Lum-A=luminal A; Lum-B=luminal B; HER2-pos= human epidermal growth factor receptor 2-positive. *P-value less than 0.05.
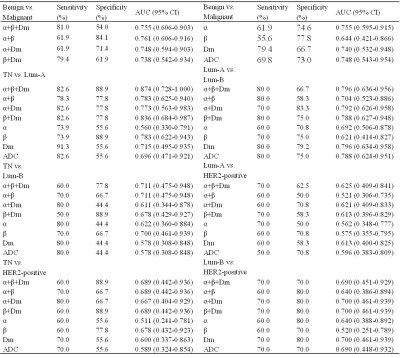
Table 3. ROC analysis of the diagnostic performance for Dm, α, β, and ADC in discriminating benign from malignant breast lesions and different molecular subtypes.
Abbreviations: TN=triple-negative; Lum-A=luminal A; Lum-B=luminal B; HER2= human epidermal growth factor receptor 2; CI = Confidence Interval.
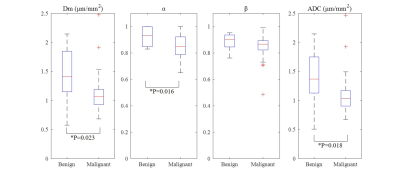
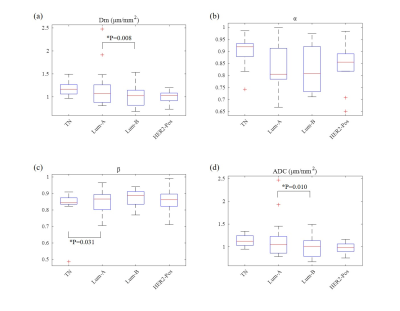
Figure 2. Box and whisker plots of mean values of the CTRW parameters, Dm (a), α (b), β (c) and ADC (d) for different molecular subtypes. Significant differences were found when comparing the parameter β in the luminal A and TN groups(p=0.031). And the luminal A had significantly higher Dm (p=0.008) and ADC (p=0.010) than luminal B. Significant findings (p<0.05) are marked with * and their corresponding p value. Abbreviations: TN=triple-negative; Lum-A=luminal A; Lum-B=luminal B; HER2= human epidermal growth factor receptor 2.