2550
Multi-shot Diffusion-weighted Imaging of the Breasts in the Supine versus Prone Position1Radiology, Stanford University, Stanford, CA, United States, 2General Electric Healthcare, Boston, MA, United States
Synopsis
Keywords: Breast, Diffusion/other diffusion imaging techniques
Diffusion-Weighted Imaging (DWI) allows for the detection of breast cancer without a contrast injection, while supine positioning may improve the comfort and efficiency of a breast MRI screening exam. This work investigates multi-shot DWI of the breasts in the supine versus prone positions, in both asymptomatic volunteers and patients with breast lesions. Supine multi-shot DWI outperformed prone multi-shot DWI based on an image quality observer study, receiving significantly higher ratings for sharpness, aliasing, and overall image quality. Lesion Apparent Diffusion Coefficients (ADCs) were highly correlated between the two positions, while fibroglandular tissue ADCs were significantly higher in the supine position.
Introduction
Despite multiple studies reporting the strength of MRI for the detection of breast cancer, it is recommended for screening in only a small percentage of women (1-3). Thus, there is interest in methods to make breast MRI more screening-appropriate, to facilitate use in a larger population of women (4). Diffusion-weighted Imaging (DWI) allows for the detection of breast cancer without a contrast injection, while supine positioning could increase the comfort and efficiency of the exam (5). Supine DWI then, has the potential to increase the accessibility of breast MRI screening by providing a non-invasive, comfortable, and efficient exam. The feasibility of supine multi-shot DWI (msDWI) was recently demonstrated in a protocol optimization study (6). In this work we investigate the performance of supine versus prone msDWI in the breasts in volunteers and patients.Methods
Asymptomatic Volunteers and ProtocolsTwenty-four asymptomatic volunteers were scanned with multi-shot MUltiplexed Sensitivity Encoding (MUSE) DWI in both the supine and prone positions (Figure 1) (7). Exams were performed on a 3T SIGNA Premier magnet (GE HealthCare, Waukesha, WI) utilizing 15 channels of a 30-channel flexible anterior array AIR coil (GE HealthCare, Waukesha, WI) (supine) or a 16-channel Sentinelle Breast Coil (Dunlee, Best, Netherlands) (prone).
Image Quality Observer Study
Three radiologists performed a blinded observer study to assess the image quality of multi-shot DWI (msDWI) in the supine and prone positions. Features of sharpness, aliasing, perceived SNR, distortion, and overall image quality were rated on a scale from one (lowest performance) to five (highest performance). Results were assessed by mixed-effects logistic regression and interobserver agreement (8).
Fibroglandular Tissue Apparent Diffusion Coefficients
In volunteers, Apparent Diffusion Coefficients (ADCs) were measured in ROIs drawn in the largest region of fibroglandular tissue in each breast, in two slices (central/superior) for each position (supine/prone). ADCs were calculated for each voxel within the ROI using a monoexponential decay model. Mean and standard deviation of the ADC were calculated and differences were assessed by position (supine vs. prone), side (left vs. right breast), and slice location (central vs. superior).
Patients and Protocol
Five patients with biopsy-proven breast lesions were recruited to undergo a research MRI which included the supine msDWI and prone msDWI acquisitions. Supine and prone msDWI protocols, scanner, and coils matched those in the supine versus prone msDWI volunteer study (Figure 1).
Lesion Apparent Diffusion Coefficients
In patients, lesions were identified based on associated clinical reports and image assessment by a radiologist with 31 years of breast MRI expertise. On the b = 800 s/mm2 images, an ROI of tissue outside of the lesion was chosen to calculate a background signal mean and standard deviation while a second ROI was drawn around the lesion. The voxels with highest signal from within the lesion ROI were segmented by removing all voxels with signal less than the mean plus 2 times standard deviation of the background signal. Mean and standard deviation of the ADCs were calculated for each segmented region and correlation between the lesion ADCs in the supine and prone positions was analyzed.
Results
Asymptomatic VolunteersImage Quality Observer Study and Fibroglandular Tissue Apparent Diffusion Coefficients
Supine msDWI images were rated significantly higher than prone msDWI images for sharpness, aliasing, and overall image quality (Figure 2). Inter-observer agreement was not significantly different between prone and supine positioning for any feature (Figure 2). Representative images from four cases are shown in Figure 3. Mean fibroglandular tissue ADCs were significantly higher in the supine versus prone position (p = 0.012). The right breast had significantly lower mean ADC than the left breast (p = 0.028) and the superior slice has significantly lower mean ADC than the central slice (p < 0.001) (Figure 4).
Patients with Breast Lesions
Lesion Apparent Diffusion Coefficients
Lesion types and maximum diameter were: invasive ductal carcinoma (IDC) mixed with DCIS (22 mm), IDC (16 mm), borderline phyllodes tumor (45 mm), benign phyllodes tumor (36 mm), and proteinaceous cyst (12 mm). Lesion ADCs were highly correlated between prone and supine positions with concordance correlation of 0.92 (95% CI: 0.70 – 0.98) and no significant difference (p = 0.53) between lesion ADCs in the two positions. Diffusion-weighted images and ADCs for the five lesions in both the supine and prone positions are shown in Figure 5.
Discussion and Conclusion
This study provided an initial assessment of supine msDWI of the breasts with respect to standard prone msDWI. As the image quality of DWI is a known limitation for the detection of breast cancer, the significantly higher ratings of supine msDWI for three of five image features is a notable finding. Agreement of ADCs between the two positions was variable, with lesion ADCs highly correlated, but fibroglandular tissue ADCs significantly higher for supine versus prone. However, all lesion and fibroglandular tissue ADCs fell within previously reported ranges for these tissues (9-12). Overall, the results of this study are very encouraging for the continued investigation of supine msDWI in the breasts, particularly as the development of a comfortable, efficient, and noninvasive exam could facilitate the expansion of screening MRI to a wider population of women.Acknowledgements
We gratefully acknowledge research support from GE Healthcare, recruitment support from Karla Epperson, and the following funding sources: NIH/NIBIB R01 EB009055 and NIH/NCI R01CA249893.References
1. Kuhl CK, Strobel K, Bieling H, Leutner C, Schild HH, Schrading S. Supplemental Breast MR Imaging Screening of Women with Average Risk of Breast Cancer. Radiology. 2017;283:361-370.
2. Mann RM, Cho N, Moy L. Breast MRI: State of the Art. Radiology. 2019;292:520-536.
3. Monticciolo DL, Newell MS, Moy L, Niell B, Monsees B, Sickles EA. Breast Cancer Screening in Women at Higher-Than-Average Risk: Recommendations From the ACR. J Am Coll Radiol. 2018;15:408-414.
4. Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB. Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection-a novel approach to breast cancer screening with MRI. J Clin Oncol. 2014;32:2304-2310.
5. Amornsiripanitch N, Bickelhaupt S, Shin HJ, et al. Diffusion-weighted MRI for Unenhanced Breast Cancer Screening. Radiology. 2019;293:504-520.
6. Moran CJ, Middione MJ, Mazzoli V, et al. Multi-shot Diffusion-weighted Imaging of the Breasts in the Supine Position. In Proceddings of the Joint Annual Meeting ISMRM-ESMRMB, London, England. 2022:p. 4017.
7. Chen NK, Guidon A, Chang HC, Song AW. A robust multi-shot scan strategy for high-resolution diffusion weighted MRI enabled by multiplexed sensitivity-encoding (MUSE). Neuroimage. 2013;72:41-47.
8. Gwet KL. Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. 2008;61:29-48.
9. Baltzer P, Mann RM, Iima M, et al. Diffusion-weighted imaging of the breast-a consensus and mission statement from the EUSOBI International Breast Diffusion-Weighted Imaging working group. Eur Radiol. 2020;30:1436-1450.
10. Li X, Jiang N, Zhang C, Luo X, Zhong P, Fang J. Value of conventional magnetic resonance imaging texture analysis in the differential diagnosis of benign and borderline/malignant phyllodes tumors of the breast. Cancer Imaging. 2021;21:29.
11. McDonald ES, Schopp JG, Peacock S, et al. Diffusion-weighted MRI: association between patient characteristics and apparent diffusion coefficients of normal breast fibroglandular tissue at 3 T. AJR Am J Roentgenol. 2014;202:W496-502.
12. Nadrljanski MM, Milosevic ZC. Relative apparent diffusion coefficient (rADC) in breast lesions of uncertain malignant potential (B3 lesions) and pathologically proven breast carcinoma (B5 lesions) following breast biopsy. Eur J Radiol. 2020;124:108854.
Figures
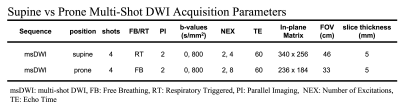
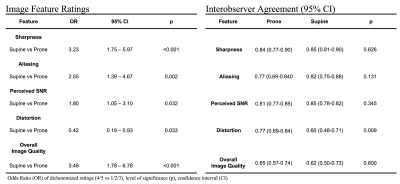
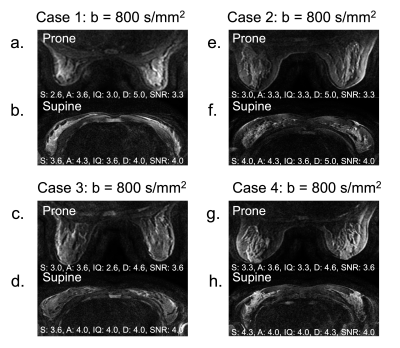
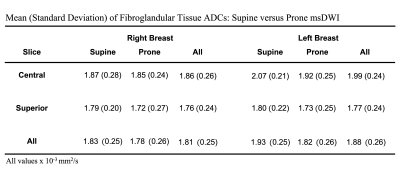

Figure 5. Prone (left column) and supine (right column) msDWI b = 800 s/mm2 images from the five (a-e) patient cases with mean (standard deviation) (x10-3 mm2/s) of lesion ADC. For all lesion types (white boxes – a: IDC/DCIS, b: borderline phyllodes tumor, c: IDC, d: benign phyllodes tumor, e: proteinaceous cyst) the lesion is discernible from the background tissue and maintains similar morphology between the two positions. The matrix was modified for the smaller FOV with prone positioning to keep prescribed resolution equivalent between the two positions.