2525
Efficacy of virtual reality therapy using functional connectivity and structural measures in children with cerebral palsy1Department of NMR, All India Institute of Medical Sciences, New Delhi, India, 2Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India, 3Center for BioMedical Engineering, Indian Institute of Technology Delhi, New Delhi, India, 4Electrical Engineering, Indian Institute of Technology, Delhi, New Delhi, India
Synopsis
Keywords: Neuro, fMRI (task based)
Hemiparetic cerebral palsy patients were administered Virtual reality therapy (VRT) in addition to constraint induced movement therapy (CIMT) in VRT group, and CIMT alone in CIMT group in a randomised trial. Task based functional MRI of left and right fist clenching and structural data were acquired in a 3T MR scanner. Cortical thickness, gyrification (using cat12 toolbox) and functional connectivity (using conn toolbox) results revealed presence of salience and motor networks in the VRT group, highlighting better recovery mechanism stimulated by virtual reality based training.Introduction
Neuromotor impairments, resulting in impairment in strength, tone, sensory and motor control in upper limb is predominant in patients with Cerebral palsy (CP), with prevalence varying from 1.2-2.5 per 1000 live births (1,2). Asymmetric cerebral palsy accounts to 29 to 36% of cases (3,4). Activating the inactive limb to improve its performance by inhibiting the active (unaffected) limb and overcoming the learned non-use or the developmental disregard (of the affected limb) is the principle of constraint induced movement therapy (CIMT) (5-7). Virtual reality therapy (VRT) uses interactive simulations to engage in environments that appear and feel similar to real-world objects and events (8,9).The study investigated the usefulness and efficacy of VRT in improving the hand function over CIMT alone, in children with hemiparetic cerebral palsy using functional MRI (fMRI).
Methodology
Children with hemiparetic cerebral palsy (both perinatal and postnatal acquired brain injury) aged >5-18 years were recruited after informed consent from parents/guardians. An Intelligence quotient (IQ) >70 (Binet Kamat Test/Malin‘s Intelligence Scale for Children), Modified Ashworth scoring 1-3 for affected limb and preserved vision and hearing (with or without correction) were the inclusion criteria. Block randomization in 1:1 ratio with variable block size was done using computer generated random numbers, to VRT group (mCIMT + VRT) and CIMT group (mCIMT alone).Baseline functional assessment of the upper limbs was done using QUEST score/Nine Hole Peg Board Test/ Hand Held Dynamometer and quality of life by cerebral palsy quality of life-child scale (CP-QOL child).
Treatment was initiated within one week of baseline assessment, with 12 visits over the duration of intervention for supervised sessions, in each group. The control arm received only mCIMT and the intervention arm received both VRT and mCIMT (CIMT in a virtual environment) with intervention provided in a supervised manner for 2 hours per session for total 8 days over first 4 weeks, followed by 2 hours per session once a week for the next 8 weeks. VRT virtual environment was a modified play environment (nature of the tasks similar to CIMT) created using X-box and Kinect motion sensor device, and a computer, and was a non-immersive VR delivery system. Parents were advised regarding the therapy to be provided at home on these visits. Compliance log was provided to them at the first visit and was regularly monitored.
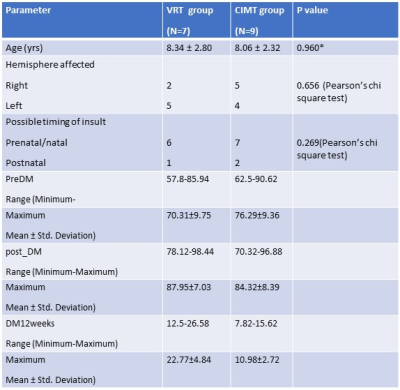
20 children were randomized to VRT group (VRT+ mCIMT) and mCIMT group. 1 patient each from intervention as well as control group, were lost to follow up within first 4 weeks of enrolment (due to family problems). They were also included in the final analysis (Intention to treat analysis), and their baseline parameters were considered for subsequent analysis at 8 weeks and 12 weeks.
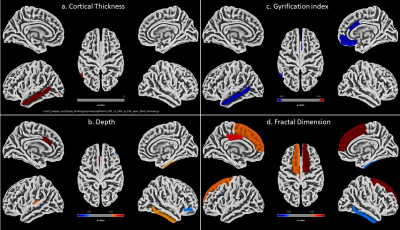
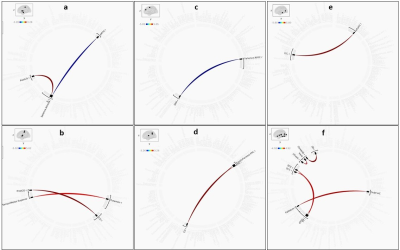
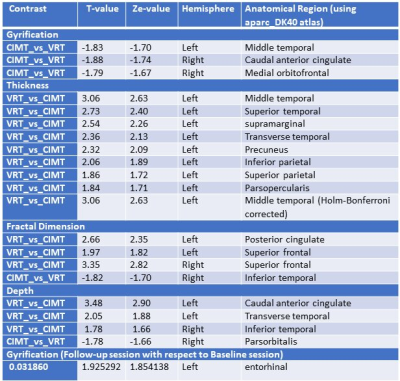
Both the intervention and control group patients were compliant throughout the study period. Structural T1 data (3D TFE, sagittal orientation, 360 slices of 1mm slice thickness) and motor task based functional MRI (EPI sequence, 150 dynamics (5 blocks of rest (30s) and active (fist clenching at a frequency of ~1Hz for 30s) cycles, 31 slices 4mm thickness, no slice gap, TR/TE:2000/30 ms) was acquired in 7 patients in VRT group (VRT+ mCIMT) and 9 patients in CIMT group, both at baseline and follow up (8 weeks), on a 3T MR scanner (Ingenia 3.0T, M/s. Philips HealthCare, The Netherlands) using 32-channel head coil. T1 data were processed using CAT12 toolbox and task based functional data using CONN toolbox (ver 21a) using standard pipeline. Results were evaluated with a p value of <0.05 uncorrected (if not significant at Holm-Bonferroni corrected) for T1 and pFDR=0.05 for fc data.
Results
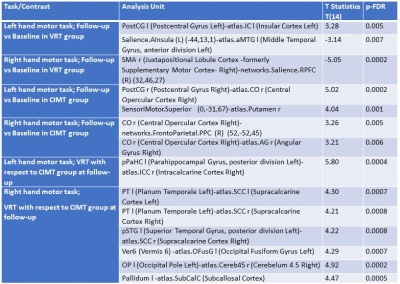
There was no statistically significant difference in any of the baseline demographic and clinical characteristics (Table 1). The mean age of the study population was 8 years in both the groups. Quest scores was significant in the VRT group at 8 and 12 weeks (U=2, p asymptotic 2 tailed=0.002). The structural measures revealed an increase in the cortical thickness, depth and fractal dimensions and a decrease in the gyrification index in the VRT group as compared to CIMT group (Table 2) at a p value of <0.05 uncorrected. Only left cerebral middle temporal cortex was observed to be highly significant at Holm-Bonferroni corrected. Left cerebral entorhinal cortex was significant on gyrification at follow-up session in comparison with that in baseline. Functional connectivity between follow-up and baseline in VRT group revealed memory, language and motor networks for left and right hand task (Table 3). Comparison of VRT with respect to CIMT group revealed attention, language and visual networks (Table 3).Discussion
Structural parameters have revealed changes with time/intervention (10-12). Our results exhibited a significant change in left cerebral middle temporal cortex on thickness and left cerebral entorhinal cortex on gyrification suggesting its implications in recovery of memory and language aspects. Functional connectivity of task based BOLD data revealed presence of salience and motor networks at follow-up with respect to the baseline in the VRT group, highlighting better recovery mechanism stimulated by virtual reality based training.Conclusion
Virtual reality based training is superior to the constraint induced movement therapy.Acknowledgements
No acknowledgement found.References
1. Paneth N,Hong T,Korzeniewski S. The descriptive epidemiology of cerebral palsy.Clin Perinatol.2006 Jun;33(2):251–67
2. Oskoui M, Coutinho F, Dykeman J, Jetté N, Pringsheim T. An update on the prevalence of cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol. 2013 Jun;55(6):509–19
3. Johnson null. Cerebral palsies: epidemiology and causal pathways. Arch Dis Child. 2000 Sep;83(3):279A.
4. Beaman J, Kalisperis FR, Miller-Skomorucha K. The infant and child with cerebral palsy. In: Tecklin J, ed. Pediatric physical therapy 5 ed. Sydney: Lippincott Williams & Wilkins; 2015:187–246
5. Taub E, Ramey SL, DeLuca S, Echols K. Efficacy of constraint-induced movement therapy for children with cerebral palsy with asymmetric motor impairment. Pediatrics. 2004 Feb;113(2):305–12.
6. Sakzewski L, Ziviani J, Abbott DF, Macdonell RAL, Jackson GD, Boyd RN. Equivalent retention of gains at 1 year after training with constraint-induced or bimanual therapy in children with unilateral cerebral palsy. Neurorehabil Neural Repair. 2011 Sep;25(7):664–71.
7. Choudhary A, Gulati S, Kabra M, Singh UP, Sankhyan N, Pandey RM, et al. Efficacy of modified constraint induced movement therapy in improving upper limb function in children with hemiplegic cerebral palsy: a randomized controlled trial. Brain Dev. 2013 Oct;35(9):870–6
8. Laver K, George S, Thomas S, Deutsch JE, Crotty M. Cochrane review: virtual reality for stroke rehabilitation. Eur J Phys Rehabil Med. 2012 Sep;48(3):523–30.
9. Sangani, S., et al. Development of a complex ecological virtual environment. in Proceedings of the 9th International Conference on Disability, Virtual Reality and Associated Technologies, Laval, France.(2012)Sept: 10–12
10. Bonkhoff AK, Hong S, Bretzner M, et al. Association of Stroke Lesion Pattern and White Matter Hyperintensity Burden With Stroke Severity and Outcome. Neurology. 2022 Sep 27;99(13):e1364-e1379. doi: 10.1212/WNL.0000000000200926.
11. Qu JF, Zhou YQ, Liu JF, et al. Right Cortical Infarction and a Reduction in Putamen Volume May Be Correlated with Empathy in Patients after Subacute Ischemic Stroke-A Multimodal Magnetic Resonance Imaging Study. J Clin Med. 2022 Jul 31;11(15):4479. doi: 10.3390/jcm11154479.
12. Tao J, Li Z, Liu Y, Li J, Bai R. Performance Comparison of Different Neuroimaging Methods for Predicting Upper Limb Motor Outcomes in Patients after Stroke. Neural Plast. 2022 Jun 6;2022:4203698. doi: 10.1155/2022/4203698.
Figures