2521
Cortical morphology-based prediction of communication disorder in children with bilateral spastic cerebral palsy1Department of Radiology, the Affiliated Hospital of Zunyi Medical University, zunyi, China, 2Department of Radiology and Nuclear Medicine, Xuanwu Hospital, Capital Medical University, beijing, China, 3Department of Radiology, Mianyang Hospital of T.C.M, mianyang, China, 4Department of Radiology, Chongqing University Central Hospital,, chongqing, China
Synopsis
Keywords: Neuro, Brain
This study were preliminarily established an individualized diagnosis model of communication dysfunction in children with bilateral spastic cerebral palsy based on cortical morphological parameters extracted from structure magnetic resonance images by using Support Vector Machines classification algorithm. This may provide a novel idea for the diagnose of communication disorder in children with BSCP.Introduction
Cerebral palsy (CP) is the most common disabling disorder in children and the bilateral spastic cerebral palsy (BSCP) subtype is the most prevalent[1]. The communication dysfunction are common problems in children with BSCP, which severely affect their learning ability and their future career progression. The intervention begins as earlier as possible, communication function of children with BSCP can be improved[2-4]. Thus, it is essential to identify the children with communication disorder in pediatric BSCP. This study aimed to seek effective neuroimaging biomarkers for the individual diagnosis of communication disorder of BSCP children.Methods
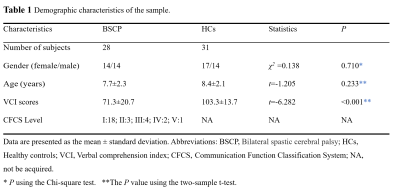
The study finally included 59 subjects (28 children with BSCP and 31 healthy controls [HCs])(Table 1). The inclusion criteria for the case group were as follows: (1) clinically diagnosed BSCP; (2) age 4-16 years at the time of magnetic resonance images (MRI) scanning; (3) MRI indicates periventricular white matter lesions(the most common type of injuries among the BSCP). The exclusion criteria were: (1) any other neurological disorders and/or history of malignant tumors or head trauma; (2) image artifacts affecting the image analysis. MRI were acquired on a 3 T scanner (Signa HDXT; GE Healthcare, Milwaukee, Wisconsin) with an 8-channel head coil. High resolution structure images were acquired using three-dimensional T1-weighted imaging(3D-T1WI) sequence with the following parameters: repetition time (TR)/echo time (TE)=7.8/3.0ms, slice thickness =1mm, field of view(FOV) =256×256 mm2, matrix =256×256, flip angle =15°. Verbal comprehension index (VCI) of Wechsler Intelligence Scale for Children 4nd edition were performed in children with BSCP and healthy controls. Communication Function Classification System (CFCS) was assessed in children with BSCP.Based on the FreeSurfer version 5.3.0 image analysis suite (http://surfer.nmr.mgh.harvard.edu), high resolution structure images of BSCP and healthy controls groups were processed to obtain cortical morphological parameters(cortical surface area, cortical volume, and subcortical structures volume) using the Destrieux Atlas. Then, with these features, Support Vector Classification (SVC) algorithm was used to construct a prediction model to predicted whether the children with BSCP have communication disorder, and the CFCS level of I is defined as communication function normally, and the CFCS level of II-V is defined as communication disorder. Feature dimensionality reduction was achieved using two-sample t-test(the BSCP and control groups were compared). Receiver operating characteristic curve was used to evaluate model performance. Leave-one-out cross-validation is applied to test the classification capability of the prediction model constructed by SVC, and for the assessment of the statistical significance of classification accuracy, non-parametric permutation tests were adopted, P < 0.05 considered to be statistically significant difference. Feature contributions from different gyrus in the model passed a permutation test were quantified by normalized feature contribution weights which were projected back on a cortical surface for visualization.
Cortical morphological parameters were also compared between the two groups using two-sample t-test. Spearman rank correlation were applied to compute the correlation between significantly different cortical morphological parameters among two groups and VCI as well as CFCS levels, considering age and sex as a covariate, and P < 0.05 considered to be statistical significance, multiple comparisons were corrected using the Bonferroni method.
Results
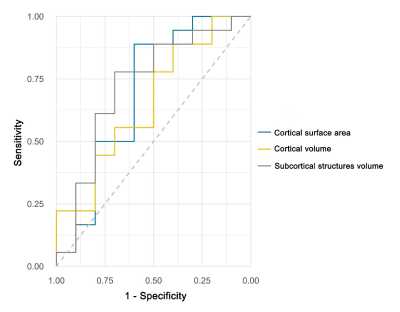
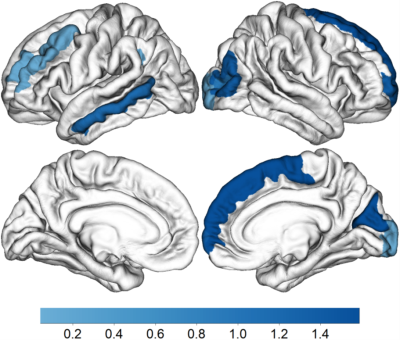
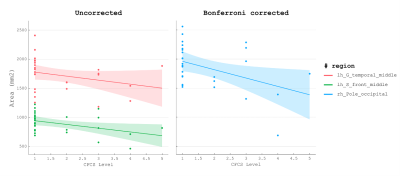
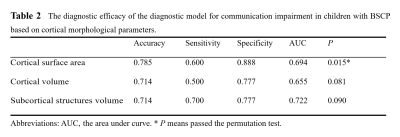
The accuracy of using cortical morphological parameters (cortical surface area, cortical volume, and subcortical structures volume) as characteristic information to distinguish whether children with BSCP had combined communication disorder was 78.5%, 71.4%, and 71.4%, respectively. And the reliability of the constructed model based on cortical surface area passed a permutation test (P = 0.015; AUC value = 0.694; Sensitivity = 0.600; Specificity = 0.888) (Table 2) (Figure 1). In this model, the features that contributed to distinguish communication disorder in children with BSCP were mainly located in the left middle frontal gyrus(L-MFG), left middle temporal gyrus(L-MTG), right superior frontal gyrus(R-SFG), right frontopolar transverse gyrus/sulcus, right middle occipital gyrus(R-MOG), right cuneate gyrus (R-CG), and right occipital pole (R-OP) (Figure 2).The cortical surface area of the L-MTG, L-MFG and R-OP were negatively correlated with CFCS, the correlations (r values) ranged between -0.389 and -0.452, and the P-values range between 0.020 and 0.049(Figure 3). And the distribution of these brain regions were consistent with the location of features that contributed to distinguish communication impairment in children with BSCP.
Conclusion
The cortical surface area could be used to establish an individualized diagnostic model of communication disorder in children with BSCP, which may provide a new way to diagnose communication disorder in children with BSCP, and communication disorder in children with BSCP was associated with the cortical surface area of the L-MTG, MFG and R-OP cortex.Acknowledgements
NoneReferences
[1]. Patel, D. R.; Neelakantan, M.; Pandher, K.; Merrick, J., Cerebral palsy in children: a clinical overview. Transl Pediatr 2020, 9 (Suppl 1), S125-S135.
[2]. Van Naarden Braun, K.; Doernberg, N.; Schieve, L.; Christensen, D.; Goodman, A.; Yeargin-Allsopp, M., Birth Prevalence of Cerebral Palsy: A Population-Based Study. Pediatrics 2016, 137 (1).
[3]. Kristoffersson, E.; Dahlgren Sandberg, A.; Holck, P., Communication ability and communication methods in children with cerebral palsy. Dev Med Child Neurol 2020, 62 (8), 933-938.
[4]. Pennington, L.; Dave, M.; Rudd, J.; Hidecker, M. J. C.; Caynes, K.; Pearce, M. S., Communication disorders in young children with cerebral palsy. Dev Med Child Neurol 2020, 62 (10), 1161-1169.
Figures