2496
Hyperpolarized 129Xe Magnetic Resonance Imaging in Patients with Brain Tumors1Department of Radiology, Chinese PLA General Hospital, Beijing, China, 2School of Medical Imaging, Guizhou Medical University, Guiyang, China, 3Key Laboratory of Magnetic Resonance in Biological Systems, State Key Laboratory of Magnetic Resonance and Atomic and Molecular Physics, National Center for Magnetic Resonance in Wuhan, Wuhan Institute of Physics and Mathematics, Innovation Academy for Precision Measurement Science and Technology, Chinese Academy of Sciences-Wuhan National Laboratory for Optoelectronics, Wuhan, China
Synopsis
Keywords: Tumors, Hyperpolarized MR (Gas), Xenon-129
This study explored the application of hyperpolarized 129Xe (HP 129Xe) MR imaging in patients with brain tumors. HP129Xe MR and 1H MR imaging was performed on three subjects. The results showed that HP 129Xe MRI has the ability to detect brain tumors, but the HP 129Xe brain MR imaging showed the lesion range was mismatched with T2 weighted image (T2WI) and arterial spin labeling (ASL)image, these are needed to be addressed in the future.Introduction
In recent years, hyperpolarized 129Xe (HP 129Xe) MR has showed great advantages in lung imaging1,2. With the HP 129Xe inhaled into the lungs, the gas can diffusely dissolve in the blood and enter the brain tissue through the circulation, then the HP 129Xe MR signal in the brain was detected3. Previous studies had demonstrated that perfusion images of brain tissue can be obtained directly by HP 129Xe MRI without biological background signal interference in healthy volunteers4. Better sensitivity can be allowed. However, it has not been reported how this signal characteristic in patients with brain tumors.Methods
In vivo imaging with HP 129Xe MR was approved from the Ethics Committee of PLA General Hospital. Three female patients which were suspected brain tumors were prospectively collected for preoperative 3 T 1H MR and HP 129Xe MR scanning. All patients signed an informed consent form prior to the examination. HP 129Xe MR scanning was performed using a 3 T multi-nuclear whole-body MR scanner [uMR780(Xe), Wuhan, China] with an in-house excitation structure orthogonal array coil (two channels). HP 129Xe was produced by the spin-exchange optical pumping (SEOP) technique using a commercial polarizer system (verImagin Healthcare, Wuhan, China)1, and the gas does of 900 mL extracted into a Tedlar bag. The available spin polarization of HP 129Xe gas was 25% approximately. Four axial images were acquired on the 20th second after the inhalation of the xenon gas during a single breath-hold. HP 129Xe MR imaging parameters at 3 T were as follows: gradient-echo pulse sequence; echo time (TE) = 2.67 msec; repetition time (TR) = 20 msec; flip angle (FA) =8°;bandwidth (BW) = 300 Hz; field of view (FOV) = 250 mm × 250mm, slice thickness = 20 mm. The four slices were acquired with a matrix size of 32 × 32. 1H MR images were acquired using a 3 T MR imaging system (Discovery 750; GE Healthcare, Milwaukee, WI, USA) equipped with a 32-channel phase array coil. Axial T2-weighted imaging (T2WI): TR / TE = 5103 / 100.5 msec; FA = 111°; FOV = 256 mm × 256 mm; matrix, 256 × 256; slice thickness = 6 mm. 3D pseudo-continuous arterial spin labeling perfusion imaging (3D p-CASL): TR/TE = 4844 / 10.5 msec; post-label delay = 2025 msec; FA = 111°; FOV = 240 mm × 240 mm;matrix, 128 × 128; slice thickness = 4 mm. Five contiguous cerebral blood flow (CBF) maps (calculated from ASL images) in the same anatomical location as the HP 129Xe brain images were added to form a projected section of thickness of 20 mm.Results
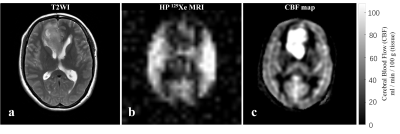
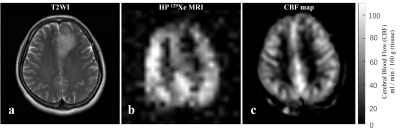
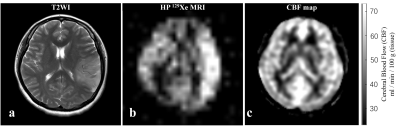
All subjects had similar reactions to the xenon dose, with slight dizziness after inhalation and breath-hold, which disappeared within 30 seconds after breath out, and no discomfort was observed for 10 minutes within finished scanning. Three cases brain images of HP 129Xe images, CBF maps, and T2-weighted 1H MR images showed in Fig1-3. Case 1: A 45-year-old female patient, right frontal lobe mass (Fig 1a), CBF map showed hyper-perfusion (Fig 1c), HP 129Xe MR image showed decreased signal in the lesion (Fig 1b), the low-signal area was more expanded than the lesion, and the low-signal area showed slightly high signal area inside. Case 2: A 49-year-old female patient, left frontal lobe mass (Fig 2a). CBF map showed no abnormality in focus perfusion (Fig 2c), while HP 129Xe MR image showed decreased signal in the lesion (Fig 2b). The range was similar to that of the T2-weighted image. Case 3: A 37-year-old female patient, the mass located in the left temporo-parietal lobes (Fig 3a). CBF map showed slightly hyper-perfusion (Fig 3c); HP 129Xe MR image showed significant hypersignal in the lesion (Fig 3b), with a larger lesion range than that of T2-weighted image.Discussion
This study shows that HP 129Xe MRI has the ability of detecting lesions in patients with brain tumors. However, HP 129Xe MRI shows abnormal signal areas which is inconsistent with the lesion. This may be a combination of multiple factors. First, because of the mass location, that can alter the normal cerebral blood flow in the area, lead to hemodynamics change in the area of tumor and peritumor, which would affect the uptake of Xe by brain tissue; Second, different types of brain tumors, which have different pathophysiological alterations, that can also produce different perfusion profiles and different blood flow profiles, this may also affect the uptake of xenon by brain tissue. Nevertheless, the changing mechanism of these dynamic alterations needs further investigation, which is the subject of future research.Conclusion
In conclusion, we demonstrate the feasibility of performing HP 129Xe brain MRI in patients with brain tumors and the diagnostic potential for evaluating HP 129Xe MR images of brain tumors. This introduces a new technique for research pathophysiological changing in brain tumors.Acknowledgements
This work was supported by the National Natural Science Foundation of China (No.81825012, 81730048 and 82151309 to Xin Lou).
References
1. Li H, Zhao X, Wang Y, et al. Damaged lung gas exchange function of discharged COVID-19 patients detected by hyperpolarized Xe MRI. Sci Adv. 2021;7(1).
2. Chen S, Lan Y, Li H, et al. Relationship between Lung and Brain Injury in COVID-19 Patients: A Hyperpolarized Xe-MRI-based 8-Month Follow-Up. Biomedicines. 2022;10(4).
3.Shepelytskyi Y, Grynko V, Rao MR, et al. Hyperpolarized Xe imaging of the brain: Achievements and future challenges. Magnetic Resonance In Medicine. 2022;88(1).
4.Rao MR, Stewart NJ, Griffiths PD, Norquay G, Wild JM. Imaging Human Brain Perfusion with Inhaled Hyperpolarized Xe MR Imaging. Radiology. 2018;286(2):659-665.
Figures